Nocturnal Enuresis in children: Symptoms, Causes, Diagnosis, Treatment with homeopathic medicine
- ABSTRACT:
Nocturnal enuresis can be very embarrassing for children and their families as the child grows up, but clinical intervention usually is not required until the child reaches about 5 to 7 years of age. However, nocturnal enuresis should not be left untreated. Motivational therapy, enuresis alarms are some of the modern treatment plan foundations. Homoeopathy can play a major role in treating this condition from which a great portion of children suffer all over the world.
- KEYWORDS:
Nocturnal enuresis; children; homoeopathy.
ABBREVIATIONS:
Diagnostic and statistical manual of mental disorders (DSM- IV), monosymptomatic nocturnal enuresis (MNE), lower urinary tract symptoms (LUTS), non-monosymptomatic nocturnal enuresis (NMNE), altered antidiuretic hormone (ADH), arginine vasopressin (AVP), chronic kidney disease (CKD), thyroid stimulating hormone (TSH)
- INTRODUCTION:
Nocturnal enuresis is a widespread and distressing condition that can have a deep impact on the child/young person’s behaviour and on their emotional and social life. It is also particularly stressful for the parents or guardians. Nocturnal enuresis can affect normal daily routines and social activities. It can also generate much more serious feelings and behaviours, such as a sense of helplessness and a lack of hope and optimism, feelings of being different from others, feelings of guilt and shame, humiliation, victimization and loss of self-esteem. There is evidence that children with bedwetting have higher than average levels of oppositional behaviour and conduct problems.1
- DEFINITION:
- Nocturnal enuresis is defined as intermittent incontinence whilst sleeping.2
- The diagnostic and statistical manual of mental disorders (DSM- IV) defines nocturnal enuresis as an involuntary voiding of urine during sleep, with a severity of at least twice a week, in children aged >5 years in the absence of congenital or acquired defects of the central nervous system.1
- TYPES:
- Monosymptomatic nocturnal enuresis (MNE) is defined as nocturnal enuresis inchildren without any other lower urinary tract symptoms (LUTS) and without a history of bladder dysfunction.1 MNE accounts for <50% of children with bedwetting.2
- Non-monosymptomatic nocturnal enuresis (NMNE) includes children with associated voiding dysfunction.2
- Primary nocturnal enuresis refers to children that have never been dry for more than a 6-month period; it is the more common form, occurring in 80% of cases.3
- Secondary nocturnal enuresis refers to the re-emergence of bedwetting after a period of being dry for at least 6 months.3
- EPIDEMIOLOGY:
- The worldwide prevalence of enuresis among children aged 6-12 years is 1.4%-28%.3
- Indian data on incidence and prevalence are very limited. In general, prevalence of nocturnal enuresis is higher among male children than female children. The prevalence in India is 7.61%-16.3%. The prevalence is highest in children aged 5-8 years and lowest in children aged 11-12 years.3 The prevalence in adult is ⁓ 0.5%.2
- In rural areas in India, the prevalence is higher among children from poor socioeconomic class compared to those from the upper middle class. A family history of enuresis has been identified in enuretic children from both rural and urban areas.3
- PATHOPHYSIOLOGY:1,2,3
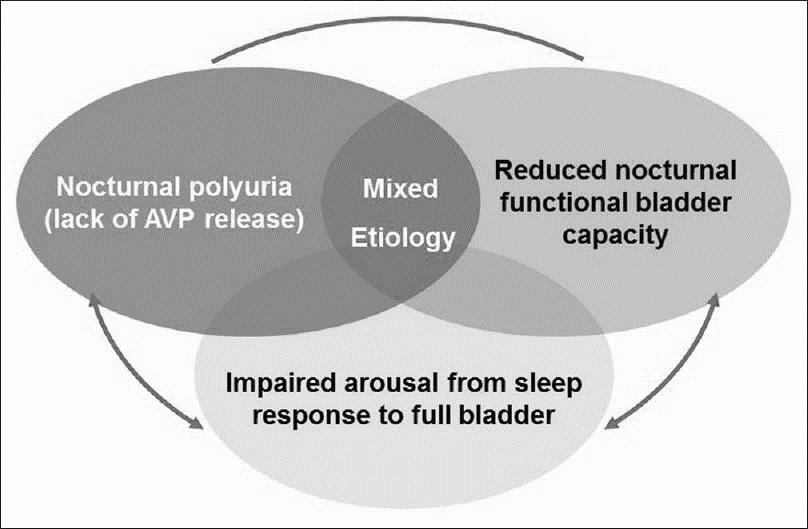
The exact cause of nocturnal enuresis is not clearly known, but several factors may be contributory. Three main factors that interact to produce nocturnal enuresis are:
- Altered antidiuretic hormone (ADH) or arginine vasopressin (AVP) secretion: an abnormal decrease in ADH levels at night causes increased urine production (nocturnal polyuria). Impaired or deficient growth hormone release may inhibit vasopressin release, causing excess urine production at night.
- Altered sleep/arousal mechanism: impaired ‘arousal from sleep’ response to a full bladder; inadequate arousal may impair secretion of vasopressin, or vasopressin deficiency may impair arousal.
- Reduced nocturnal functional bladder capacity (± nocturnal detrusor over activity): children with nocturnal enuresis have smaller functional bladder capacities and high bladder instability at night.
Genetics play a crucial role in nocturnal enuresis. Familial predisposition, psychological factors, urinary tract infection, and constipation are also considered to contribute to nocturnal enuresis.
- RISK FACTORS:3
- Living with a single parent
- Living with step-parents
- Parents with health problems
- Conflicts at home
- Stress due to enuresis
- Scolding
- Poor scholastic performance
- EVALUATION:
- HISTORY TAKING:2
Homoeopathy treats the patient, not the disease. In homoeopathic treatment, while taking a case, our main aim is to form a totality of symptoms by the process of individualisation considering past history, family history, all the generalities, and the peculiar characteristic features of the patient.
Enquiry should be made about –
- The frequency of episodes
- Whether it is a new or recurrent problem
- Daytime urinary symptoms, urgency, holding manoeuvres, daytime incontinence
- Bowel habit (constipation, incontinence)
- Any underlying contributory medical conditions
- Family history
- Psychosocial history
- CLINICAL ASSESSMENT:2,3
Physical examination in a child with MNE is usually normal. Physical examination in children with NMNE is recommended which should involve examination of the –
- Abdomen (for distended bladder and faecal impaction)
- Rectum, genitals (for signs suggestive of sexual abuse which may be the cause of secondary or persistent enuresis)
- Neurological examination
- Lower limb sensation
- Examination of the spine
- Assessment of overall growth with the help of growth chart is essential to check for growth retardation due to chronic kidney disease (CKD) or obstructive uropathy.
- INVESTIGATIONS:2,3
- Voiding diary/ Frequency-volume charts: to assess for nocturnal polyuria and functional bladder capacity; a baseline record of the enuresis pattern over 2 weeks can assess enuresis severity and give an objective measure of bladder performance. This diary records
- The time of going to bed and waking up
- Whether it was dry or wet night
- The volume of urine passed at night and in the morning
- The weight of the diaper in the morning, and
- The bowel movements
- Urinalysis: to assess for infection, the presence of glucose (diabetes) or protein (urinary tract infection, renal disease).
- Serum glucose: elevated in secondary enuresis.
- Blood urea nitrogen: elevated in secondary enuresis.
- Serum creatinine: elevated in secondary enuresis.
- Serum TSH: decreased in secondary enuresis.
- Urodynamic study: in general, not required; however, urodynamic study shows that bladder wall thickness is significantly higher in patients with detrusor over activity.
- Ultrasonography of kidney and bladder/ voiding cystourethrogram: to rule out the possibility of ectopic ureter, particularly in treatment-resistant cases; although it is rare.
- DIFFERENTIAL DIAGNOSIS:3
Renal, neurologic, and organic disease states can also cause symptoms of nocturnal enuresis.
| CONDITIONS | DIFFERENTIATING SIGNS/ SYMPTOMS | DIFFERENTIATING TESTS |
| Congenital abnormality of urinary tract | Urinary tract infections, continuous incontinence or dampness, hydronephrosis | Ultrasound of kidney and bladder; voiding cystourethrogram |
| Constipation | Faecal incontinence, hard stools, rectal bleeding | Bladder x-ray or ultrasound |
| Diabetes mellitus | Glycosuria, polyuria; possible weight loss and polydipsia | Urinalysis, fasting serum glucose, glycated hemoglobin |
| Detrusor over activity | Daytime urinary frequency, urgency; possible daytime incontinence | Urodynamics, bladder ultrasound |
| Emotional disturbance | Depression and/or defiant activity | Clinical diagnosis |
| Neurological disorder (spina bifida, epilepsy) | Epilepsy at least two unprovoked seizures and may be associated with incontinence | Electroencephalogram, radiograph, computed tomography, or magnetic resonance imaging scan |
| Urinary tract infection | Fever, dysuria, abdominal pain | Urinalysis and urine culture |
| Pediatric vesicoureteral reflux | Voiding symptoms, abdominal pain | Renal ultrasound |
| Chronic kidney disease | Increased urination especially at night, decreased urination, hematuria, puffy face or hands or feet | Renal ultra sound, urine tests, renal function test |
| Posterior urethral valve | Urethral obstruction, incontinence | Renal ultrasound |
| Neurogenic bladder | Spontaneous bladder contractions, incontinence | Uroflowmetry, Filling cystometrogram |
- MANAGEMENT:
The first step is to educate the child and parents about the condition and provide reassurance regarding spontaneous resolution (annual cure rate is 15%).3 Active treatment is usually deferred until age of 6 years and should be initiated only if non-medicinal measures fail.2
- GENERAL MANAGEMENT:2,3
- Reassurance and counselling: A combination of providing reassurance, emotional support, eliminating guilt, and rewarding the child for dry nights. Cleaning after bedwetting should not be performed as a punishment.
- Bladder training: Regular daytime toileting, emptying the bladder before bed, avoiding bladder stimulants (i.e. black-current drinks, caffeine), reduced fluid intake in the hours before sleep, waking the child on a schedule of decreasing intervals over several nights; the child is made to change clothes and bedding (if wet), and walk to the toilet if voiding is required. Adjust diet to avoid constipation and treat it with laxatives if it occurs.
- Conditioning therapy: Alarm therapy with an enuresis alarm is the most effective strategy for curing nocturnal enuresis. Enuresis alarm should be considered only when behavioural measures are unsuccessful. Enuresis alarm consists of a sensor device attached to the child’s underwear or to a mat under the bed-sheet, and an alarm placed on the bedside or attached to the child’s collar. The sensor on the device is activated when bedwetting occurs. The alarm conditions the child to sense a full bladder and awaken from sleep (60–70% successful response).
- HOMOEOPATHIC MANAGEMENT:
Whatever the name of the disease may be, homoeopathic prescription is done by framing totality of symptoms only.
However, these are some of the drugs which are frequently indicated while managing a patient suffering from nocturnal enuresis –
- Apis mellifica – incontinence at night, and when coughing, with great irritation of the parts; urine clear, straw-coloured.4
- Argentum nitricum – incontinence of urine at night and in daytime; urine passed unconsciously and uninterruptedly; too profuse flow of pale urine.5
- Belladonna – involuntary urine, night and day, in girls or scrofulous children; consequent upon paralysis of sphincter muscle; urine contains white epithelia.4
- Benzoicum acidum – enuresis nocturna (after failure of Nitr.); urine high coloured, strongly ammoniacal, irritating and smelling like that of horses; from digestive disturbances; in old people.5
- Calcarea carbonica – irritable bladder; enuresis (use 30th); urine dark, brown, sour, fetid, abundant with white sediment, bloody.6
- Causticum – involuntary in children during the first sleep; incontinence of urine day and night in cold weather; with constipation.4
- Cina maritima – involuntary at night; urine turbid, white; turns milky on standing; suitable to children troubled with worms in the intestines; restless sleep at night.7
- Equisetum hyemale – enuresis diurna et nocturna; profuse watery urine, where habit is the only ascertainable cause; especially at latter part of night.4,8
- Ferrum metallicum – incontinence more frequent in daytime than at night or floods the bed several times at night; urine light-coloured, or the ammoniacal smell of the urine; stains the linen dark; clay-coloured, yellowish sediment, adhering to the sides and bottom of the vessel.5
- Kreosotum – incontinence of urine; copious, pale; urging, cannot get out of bed quick enough; during first sleep, from which child is roused with difficulty; he dreams that he is urinating in a decent manner.5,8
- Lac caninum – frequent and profuse urination; at night she dreams of urinating, and wets the bed.5
- Medorrhinum – nocturnal enuresis; passes enormous quantity of ammoniacal, high coloured urine in bed every night; < by over-work or over-play, extremes of heat or cold, when the best selected remedy fails; with a history of sycosis.8
- Nux vomica – where the weakness has been caused by use of intoxicating drinks, and intemperate habits; paralysis of urinary bladder, urine dribbles.7
- Physalis – enuresis; nocturnal incontinence; sudden inability to hold it in women; urine acrid, foul.6
- Plantago major – urine profuse flow, nocturnal enuresis. 6
- Psorinum – during full moon; intractable cases; with eczematous history.6
- Pulsatilla nigricans – involuntary urination when coughing and during sleep; especially at latter part of night; from digestive disturbances.4,6,7
- Quassia – excessive desire – impossible to retain urine; copious micturition day and night. As soon as the child wakes up bed is drenched.6
- Rhus aromatica – enuresis due to vesical atony; constant dribbling; senile incontinence; urine pale, albuminous.6
- Rhus toxicodendron – involuntary discharges of urine at night, or while sitting, or when at rest; weakness of bladder, with constant dribbling and inconvenient desire to pass water; gouty or rheumatic subjects.5
- Santoninum – urine greenish if acid and reddish purple if alkaline; incontinence and dysuria; enuresis; feeling of fullness of bladder; chronic cystitis.6
- Sepia officinalis – child or adult wets the bed as soon as he goes to bed; always during the first sleep; urine deposits a reddish clay-coloured sediment which adheres to the vessel as if it had been burned on; foetid, so offensive must be removed from the room.5,7,8
- Silicea terra – enuresis nocturna, especially in children suffering from worms or chorea; weakness of urinary organs and constant desire to urinate; bloody, involuntary, with red or yellow sediment.5,6
- Sulphur – wetting bed at night, copious discharge; urine increased or involuntary at night; urine fetid, greasy pellicle on the surface; especially in scrofulous, untidy children.4,6,7
- Thyroidinum – enuresis in weakly children who are nervous and irritable (1/2 gram night and morning); urine smells of violets, burning along urethra, increase of uric acid.6
- Verbascum thapsus – constant dribbling; enuresis; burning urination; increase with pressure in bladder.6
- Viola odorata – milky urine; smells strong; enuresis in nervous children.6
- CONCLUSION:
This assignment is an effort to understand nocturnal
enuresis including definition, types, epidemiology, pathophysiology, risk
factors, evaluation, investigations, and differential diagnosis along with
management. There are plenty of homoeopathic medicines to treat nocturnal
enuresis cases successfully. According to the situation, conventional
treatment may be required.
- REFERENCES:
- Nocturnal enuresis the management of bedwetting in children and young people clinical guideline methods, evidence and recommendations October 2010. The National Clinical Guideline Centre at The Royal College of Physicians, 11 St Andrews Place, Regent’s Park, London, NW11 4LE. First published 2010.
- Reynard J, Brerwster S, Biers S. Oxford handbook of urology. 3rd edition. Oxford university press. Oxford. 2013: 694-95.
- Reddy NM, Malve H, Nerli R, Venkatesh P, Agarwal I, Rege V. Nocturnal enuresis in India: Are we diagnosing and managing correctly? Indian J Nephrol. 2017;27:417-26. DOI: 10.4103/ijn.IJN_288_16.
- Farrington EA. Comparative materia medica. B Jain Publishers (P) Ltd. New Delhi. 14th impression. 2012.
- Lilienthal S. Homoeopathic therapeutics. B Jain Publishers (P) Ltd. New Delhi. 1986: 178-79.
- Boericke W. Pocket manual of homoeopathic materia medica. B Jain Publishers (P) Ltd. New Delhi. 56th impression. 2016.
- Johnson ID. Johnson’s therapeutic key. World Homoeopathic links. New Delhi. 17th edition: 126-27.
- Allen HC. Keynotes and characteristics with comparisons of some of the leading remedies of the materia medica. A. B. Publications. Reprint edition. 2002.
About the authors
- Dr Koushik Bhar, M.D.(Hom.), Lecturer, Dept. of Practice of Medicine, Bengal Homoeopathic Medical College and Hospital, Asansol, West Bengal
- Dr Supriya Pramanik, M.D.(Hom.), Lecturer, Dept. of Organon of Medicine, The Calcutta Homoeopathic Medical College and Hospital, Kolkata
- Dr Prabin Kumar Shaw, M.D.(Hom.), corresponding author , Lecturer, Dept. of Homoeopathic Materia Medica, The Calcutta Homoeopathic Medical College and Hospital, Kolkata