ABSTRACT
Dyslipidaemia, particularly hypercholesterolaemia and atherogenic dyslipidaemia, have been closely implicated in the pathogenesis of coronary heart disease (CHD). Abnormalities of lipid metabolism is known to be associated with lifestyle-related diseases such as metabolic syndrome. Statins are commonly used as a conventional intervention, however being an expensive treatment and involving complications, usage of the drug is impeded. In this case, a 38-year old individual diagnosed with hypertension associated with dyslipidaemia, was managed with individualised homoeopathic medicine, Lycopodium clavatum. The intervention along with therapeutic lifestyle changes showed symptomatic relief along with lowering of the lipid values. The results were assessed with simple lifestyle indicator questionnaire (SLIQ) and measure your medical outcome profile 2 (MYMOP2) questionnaire for lifestyle changes and symptomatic changes respectively. The results from this study may be used for pilot pragmatic study with robust outcome measures and larger sample size.
Keywords
Dyslipidaemia, individualised homoeopathic medicine, Lycopodium clavatum, therapeutic lifestyle changes.
Abbreviations
CVD (cardiovascular disease), NCEP (national cholesterol education program), BMI (basal metabolic index), WC (waist circumference), TDS (thrice a day), TLC (therapeutic lifestyle changes), MYMOP (measure yourself medical outcome profile), SLIQ (simple lifestyle indicator questionnaire), mg/dL (milligram per decilitre), OPD (outpatient department), IPD (in-patient department), kg (kilogram), mm Hg (millimetre of mercury), cm (centimetre).
Introduction
The major cause of death according to the recent census is cardiovascular diseases (CVD). Out of the various risk factors, dyslipidaemia is having a significant relationship with the cardiovascular diseases.1 Dyslipidaemia refers to derangements of one or many of the lipoproteins; elevations of total cholesterol, low density lipoprotein (LDL) cholesterol and/or triglycerides, or low levels of high-density lipoprotein (HDL. The term ‘atherogenic dyslipidaemia’ denotes a combination of elevated triglycerides, small-dense LDL particles, and low levels of HDL- cholesterol2.
The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) reinforces LDL as the primary target of cholesterol‑lowering therapy with the optimal goal of its level below 100 mg/dL. The panel recommends treatment beyond LDL lowering for patients with triglyceride levels of 200 mg/dL and above. Non‑HDL‑cholesterol, representing the sum of all atherogenic lipoproteins, has been identified as a secondary target of therapy in patients with elevated triglyceride levels. Managing and monitoring non‑HDL– cholesterol level is found particularly important for asian Indians3,4. Lifestyle changes such as maintenance in regular aerobic physical activity, increase intake of Omega ‑3 polyunsaturated fatty acids in diet, and therapeutic interventions such as statins (HMG‑CoA reductase inhibitors), fibrates, or a combination of statins with fibrates or niacin have been suggested for their beneficial role in lowering LDL‑cholesterol levels, TGL, and increasing HDL‑cholesterol levels, but with their adverse effects. 3
According to the National Cholesterol Education Programme Adult Treatment Panel III4
“Dyslipidaemia is defined by the presence of high total cholesterol (≥ 200 mg/dl), high LDL cholesterol (≥ 130 mg/dl), low HDL cholesterol (< 40 mg/dl), high non-HDL cholesterol (≥ 160 mg/dl), high cholesterol remnants [very low density lipoprotein cholesterol = total – (HDL+LDL) cholesterol ≥ 25 mg/dl] or high triglycerides (≥ 150 mg/dl) High total to HDL cholesterol was defined when ratio was either ≥ 5.0 or ≥ 4.0 as reported in an earlier study from India.4
The statins have been prescribed by the conventional school as the first line of treatment, but the statins have its own side effects of causing myalgia and myositis, that leads to low adherence to statins therapy. Dyslipidaemia, being asymptomatic disease, have been ignored by clinicians and the researches. With a few clinical and preclinical researches, the need of the hour is to hold researches to combat the silent killer. This study has been taken to add clinical evidence to the literature so that similar study can be taken for future control trials.
Materials and methods
Case profile
A 38-year-old female patient visited OPD of Dr. MPK Homoeopathic Medical College, Hospital and Research Centre on 12/02/2018 with OPD/IPD number 10773/2699.
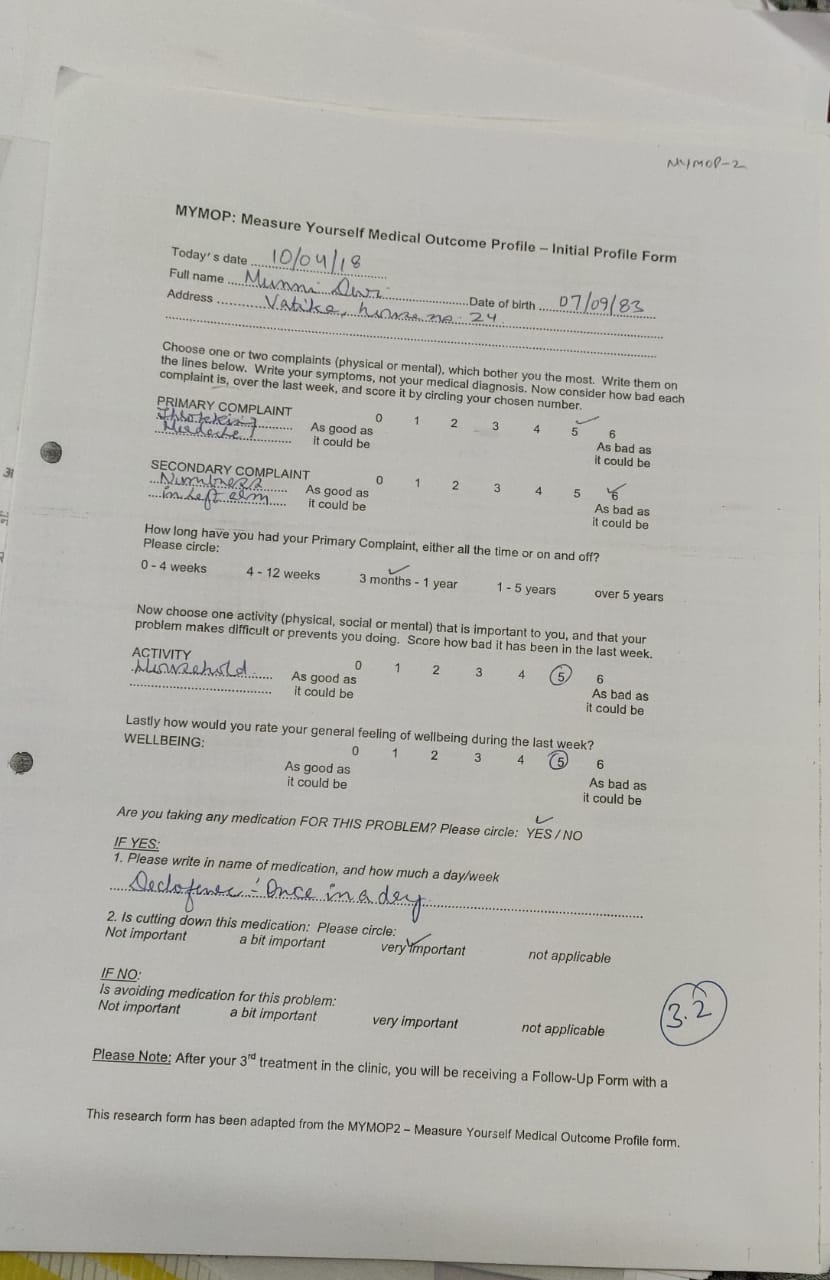
- Patient had severe throbbing headache at the temporals, aggravated with stress, slight better after bitter vomiting for 6 months.
- For 2 months, she was suffering from numbness in the left arm with formication, heaviness in arm aggravates on hangingit, slightly better when at rest.
History of presenting complaints:
The patient was apparently well 6 months back when she had severe headache, occasionally she experienced epistaxis followed with headache. She took allopathic medications that initially relieved the epistaxis, but the headache reappeared.
After a few months, she had pain with numbness in the left arm that gradually increased in intensity. She massaged with ayurvedic oil that slightly relieved the pain, but numbness persisted.
Past history: Five years back, she undertook cholecystectomy for multiple gall stones.
Personal history: The patient was an entrepreneur by profession. She was a vegetarian. She had divorce two years back and was a parent to two children.
Family history –The patient’s father was hypertensive and mother, a diabetic.
Gynaecological history-The patient was frequently suffering with urinary tract infection in the past for which she undertook allopathic treatment with relief in the complaints. She had a regular menstrual cycle with partly clotted discharges.
Physical generals: She had an endomorphic appearance. Her appetite and thirst were normal with three meals and 2-3 litres of water respectively. She had desire for sour and sweets that was not so significant. She was sensitive to hot weather, with sour smelling sweat on her palms and soles, though general complaints were better on wrapping. She had unrefreshing sleep, frequently dreaming of flying in air.
Mental generals:Angry easily; suppressed emotions, desired for company, did not want to stay alone.
Miser for her belongings, did not want to share it.
General examination:
Height-150 cm; blood pressure-135/95 mm Hg; weight-72 kg; obesity +; BMI-32 (normal < 23)
WC-32 inches; xanthelasma – absent
Investigations:
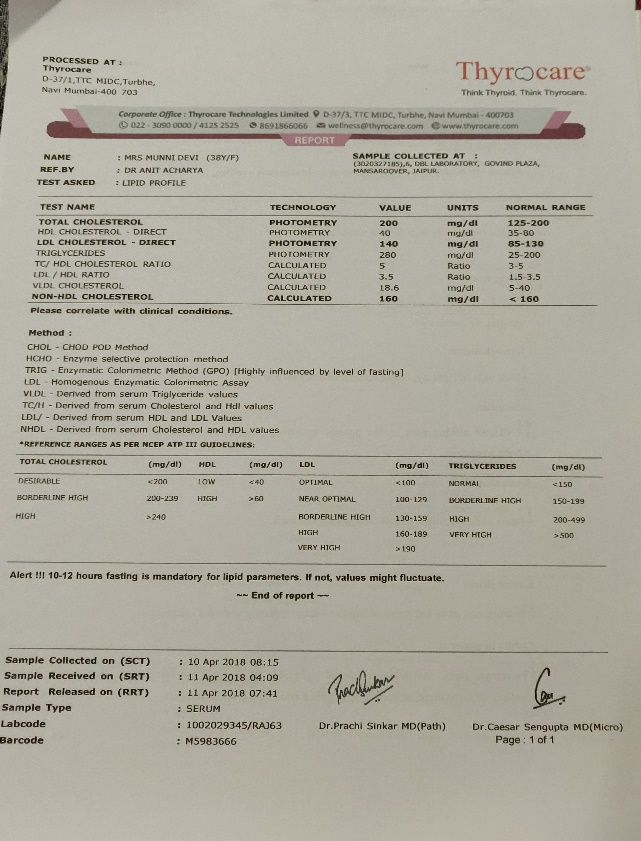
| Previous Investigations and reports |
| 10/04/18:TC 200mg/dL; TGL- 280mg/dL; HDL -40 mg/dL; LDL 140 mg/dL, non-HDL -160 mg/dL. |
Analysis and evaluation:
| S. No. | Type of symptoms | Symptoms | Intensity |
| 1. | Mental generals | Angry easily | ++ |
| 2. | Mental generals | Dreams of flying | ++ |
| 3. | Mental generals | Desire for company | ++ |
| 4. | Physical generals | Hot patient | ++ |
| 5. | Physical generals | Sour sweat on palms | ++ |
| 6. | Particulars | Throbbing headache at temporals, gets relief with vomiting | ++ |
| 7. | Particulars | Vertigo in morning on rising. | ++ |
| 8. | Particulars | Formication in left arm. | ++ |
MIASMATIC DIAGNOSIS5
Hot patient – syphilis
Desires company – psora
Angry easily – psora
Vertigo on rising – psora
Sour perspiration – psora
Formication in left hand – psora
Predominant miasm – psora
Prescription
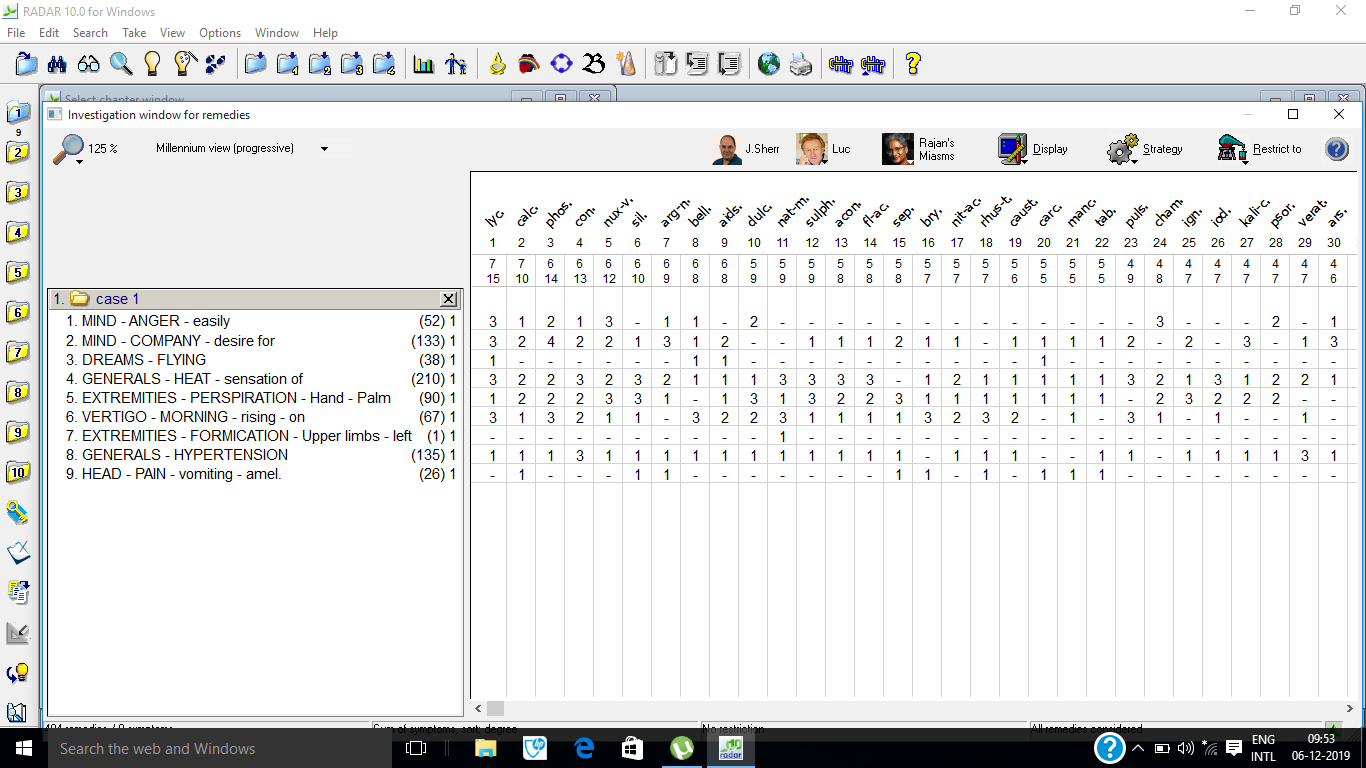
Lycopodium clavatum 15/7, Calcarea carbonicum 10/7, Phosphorus 6/14, Conium maculatum 6/13 and Nux vomica 6/12 were the top five remedies that came after repertorisation. Lycopodium clavatum covered all the symptoms with highest gradation, miasmatic background and general symptoms of the patient. Lycopodium clavatum 200 C twice a day on first day, to be taken empty stomach on clean tongue, followed by rubrum 200 thrice a day for two weeks. The potency was selected according to the nature of the case and the susceptibility of the patient.6 In Kent’s Lesser writings also, Master Kent has mentioned that a single, well selected medicine can be repeated every four hours.7
Repertorisation-Since the analysis and evaluation constituted marked physical and mental generals and particular symptoms, repertorisation was done using Synthesis Repertory. Method RADAR 10.0 FOR WINDOWS. 8
Follow up
| Date | Signs and symptoms | Prescription |
| 12/04/2018 | Headache at temporal region, with slight relief with wrapping up. Numbness and tingling in left arm, pain aggravates on hanging. Vertigo on rising in morning. BP 135/95 mm hg.The investigation showed increase in total cholesterol Triglyceride, LDL and VLDL. | Lycopodium clavatum 200C, two doses on the first day followed by placebo 30 C TDS. TLC were being advised for two weeks. |
| 24/04/18 | Headache slight better, numbness persists. Vertigo with no relief. BP 140/95mm Hg. | Rubrum 30 C thrice a day and TLC were being advised for two weeks. |
| 08/05/18 | Headache decreased in intensity slightly, numbness persists. BP 130/90 mm Hg | Placebo TDS for two weeks. TLC were being advised |
| 22/05/18 | Vertigo slight better, no improvement in numbness BP 130/90 mm Hg | Placebo 30 TDS for one month. TLC were being advised |
| 22/06/18 | Epistaxis appeared with the headache. Numbness slight relieved. BP 130/90 mm Hg | Lycopodium clavatum 200C two doses on the first day followed with Placebo 30 TDS for two weeks, advised to lower the salt content in the diet, Practice meditation. . |
| 06/07/18 | Vertigo better, no reoccurrence of epistaxis. Numbness same as before. BP 130/90 mm Hg | Placebo30 TDS for one month. TLC were being advised |
| 09/08/18 | Headache decreased with numbness and vertigo persisting. BP 120/85 mm Hg | Placebo TDS for a month. TLC were being advised |
| 10/09/18 | Symptoms slight reduced in intensity; patient is getting sound sleep. Patient advised to get the lipid profile done on the next visit. BP 130/85 mm Hg | Placebo TDS for two weeks. TLC were being advised |
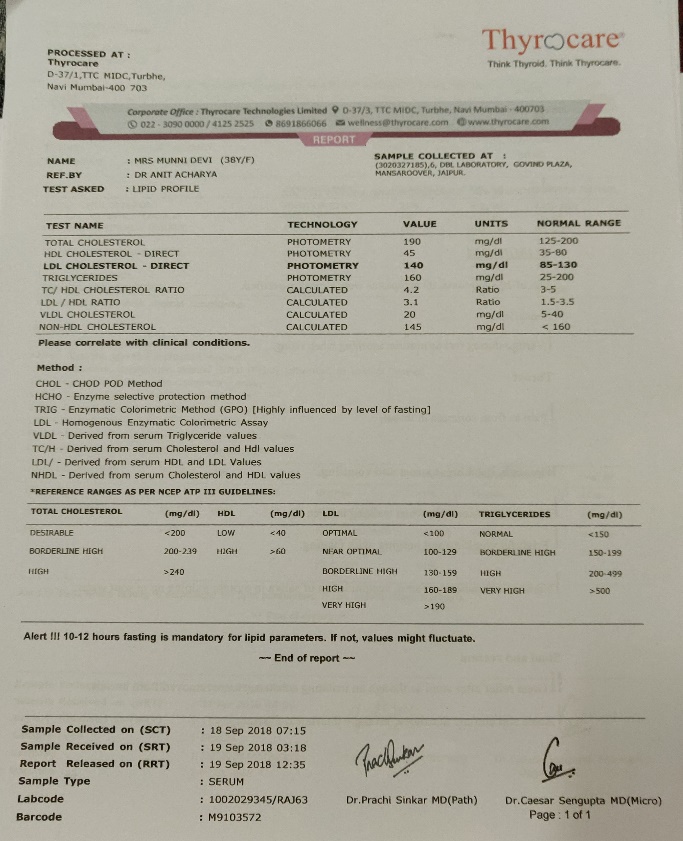
| 18/09/18 | Complaints better. The investigation showed decrease in the lipid profile. | Placebo 30 TDS for 30 days. TC 190mg/dl TGL 160mg/dl LDL 140 mg/dl HDL 45 mg/dl Non-HDL 145 mg/dl |
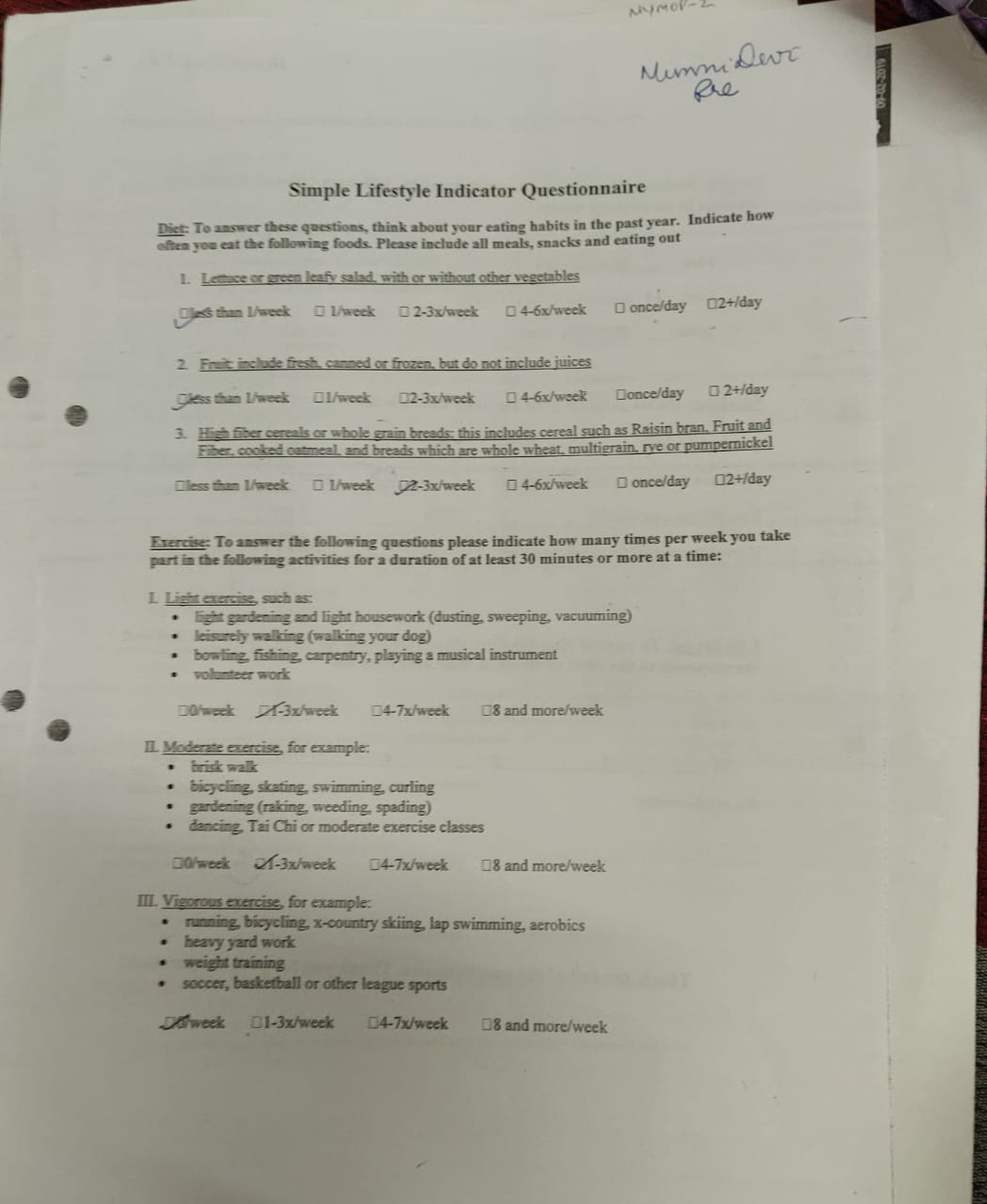
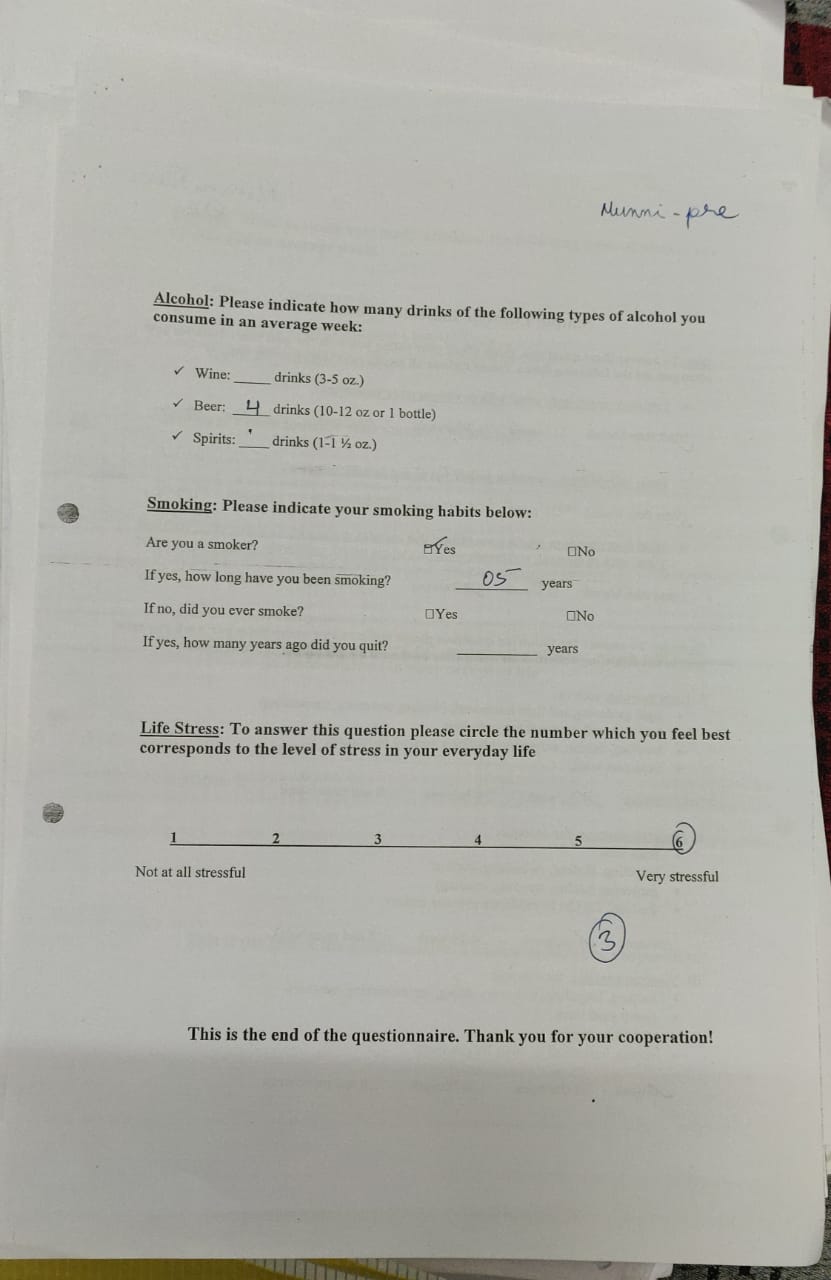
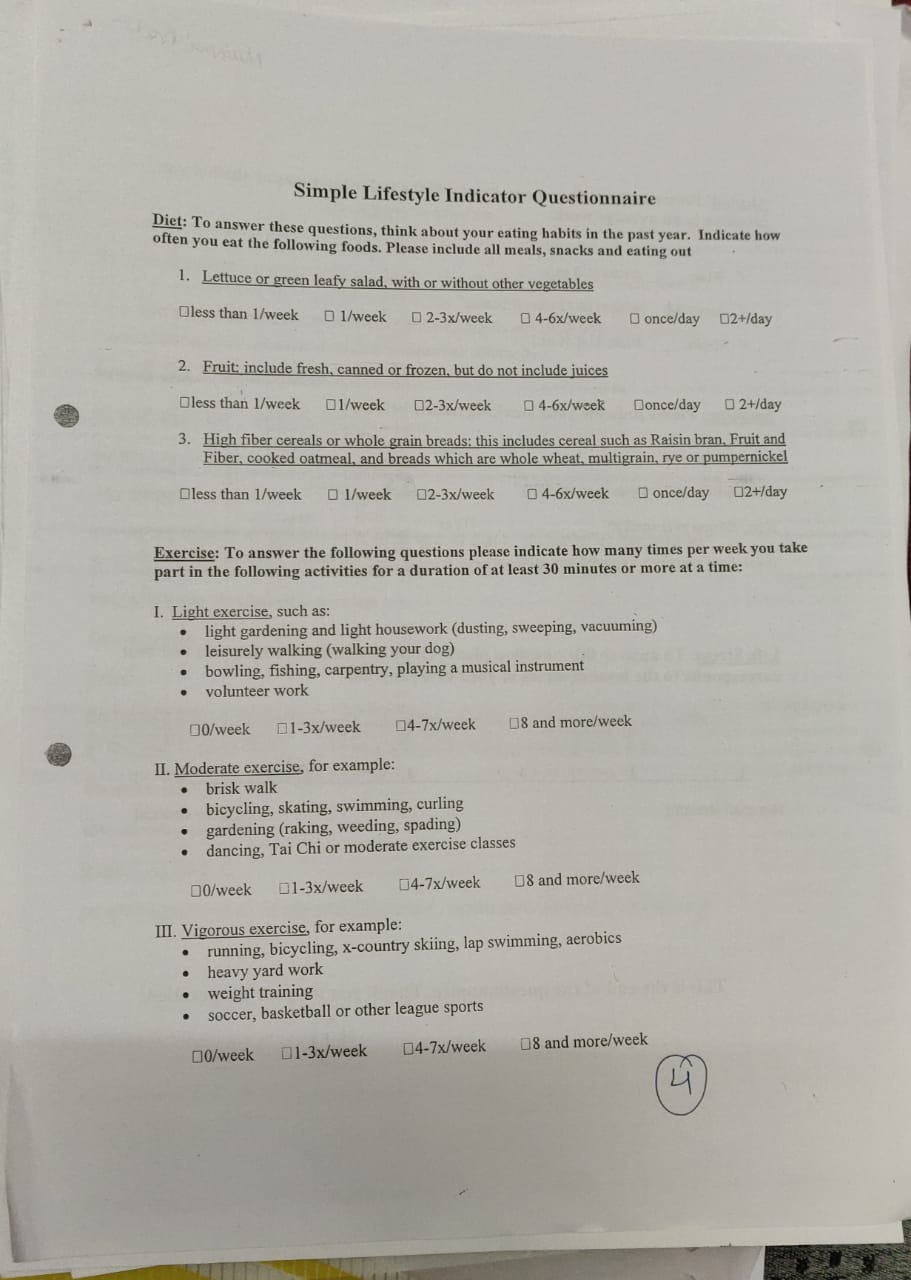
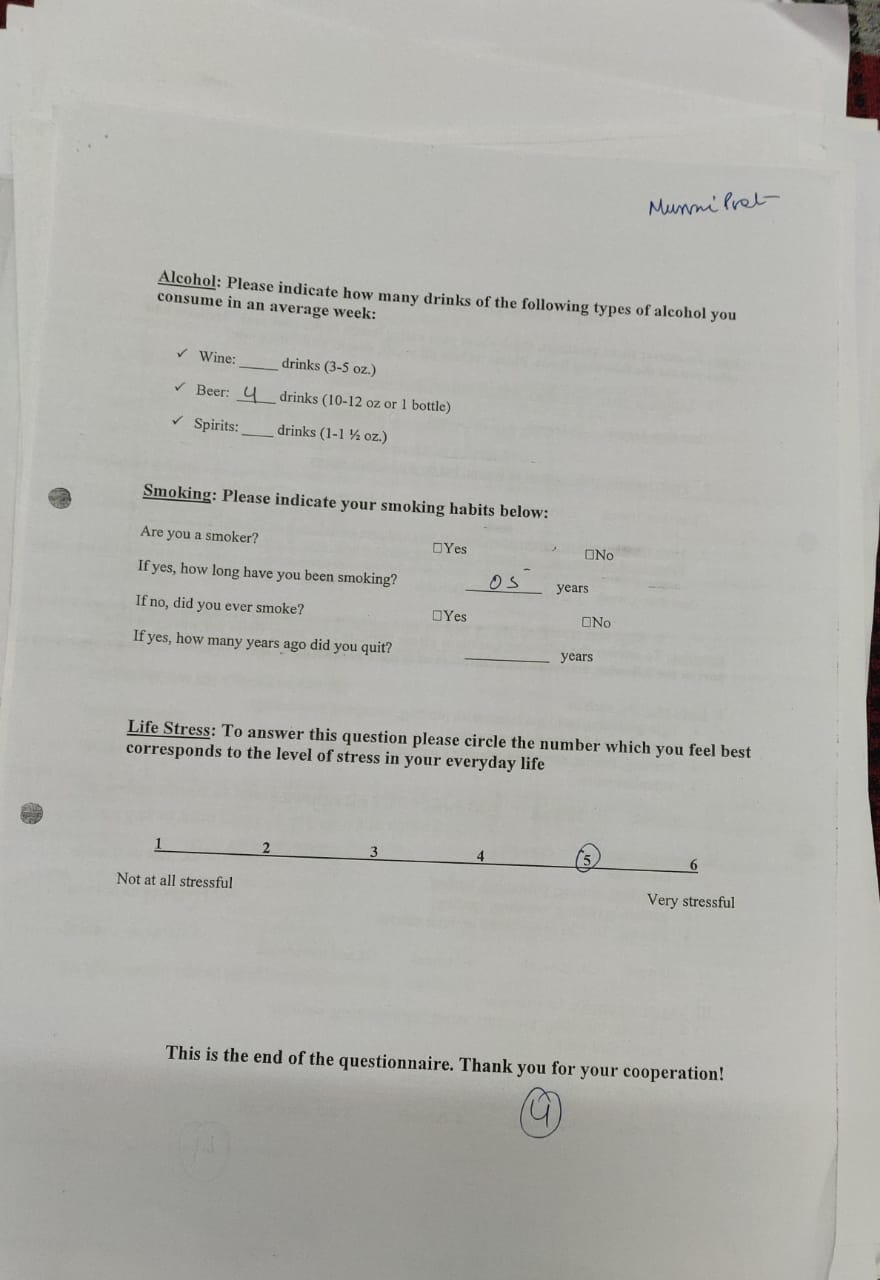
The MYMOP and the SLIQ questionnaire showed slight changes with the intervention. The MYMOP showed symptomatic changes from 3.3 to 3, while the SLIQ to assess the lifestyle modification showed change from 3 to 4. Though the changes were slight but showed the effectiveness of homoeopathic treatment along with therapeutic lifestyle changes in management of lifestyle disorders .
Concomitant therapy3–
Brisk walking for at least 30-40 minutes each day.
Practice yoga and meditation
Avoid oily rich food.
Take fibre rich diet.
Eat small and frequent meals every day.
Discussion
This case study shows the effectiveness of homoeopathy in lifestyle disorders. This single report has similar results as shown in a previous research conducted that shows the importance of MNT (medical nutritional therapy) on plasma lipoproteins of type 2 dyslipidaemic patients9.Our single case report also showed the individualised homoeopathic medicines with the therapeutic lifestyle changes as an auxillary treatment is quite helpful in the management of cases with lifestyle disorders, this also shows similar result as conducted in research conducted by CCRH.10The various literatures of materia medica11,12,13 also agreed with the repertorial totality like company desire, angry easily, hot patient and sour perspiration on palms and soles.
Conclusion
A single case report results cannot be generalised yet the outcome of this case report may improve the knowledge of the clinicians which will ultimately benefit the patients suffering from dyslipidaemia. This was a retrospective study involving a single case. So, a prospective research study with randomised controlled trial (RCT) study design is suggestive.
References
- WHO Global Status Report On NCD 2014.(Document On Internet) .Geneva ; Cited On 2017 Oct 12 Available From http://apps.who.int/iris/bitstream/10665/148114/1/ 9789241564854_eng.pdf?ua=1
- Bhalerao RD, Manchanda RK, Roja V. Homoeopathy in The Management of Dyslipidemia: A Short Review. Indian J Res Homoeopathy 2015;9(4):258-66.
- Supplement To Journal Of The Association Of Physicians Of India. Lipid Association Of India Expert Consensus Statement On Management Of Dyslipidemia In Indians 2016: Cited On 2017 Oct 22 . Available From http://www.japi.org/march_2016_special_issue/01_lipid_ association_of.pdf
- Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults. Executive Summary of The Third Report of The National Cholesterol Education Program NCEP (Adult Treatment Panel III). JAMA 2001; 285:2486-97.
- Hahnemann S. Organon Of Medicine.5thEdition. NewDelhi: B Jain Publishers Pvt Ltd;2007
- Speight P.A comparison of the chronic miasms TBS The Book Service Ltd (1 January 1961.
- Kent J T. Lectures Of Homoeopathic Philosophy.New Delhi: B Jain Publishers Pvt Ltd ;2008.
- Schroyens F. Synthesis. 7th ed. New Delhi: B. Jain Publishers Pvt Ltd;1997.
- Saha et al. Effects Of Medical Nutrition Therapy On Plasma Lipoproteins Of Type Ⅱ Dyslipidemic Patients: A Short-Term Pilot Study.Asian J Pharm Clin Res, Vol5, Suppl 4, 2012, 207-211
- Govekar JP, Paul VK, Singh K, Oberai P, Roja V. Hyperlipoproteinemia. Clinical Research Studies – Series II: New Delhi: CCRH; 2009. p. 63-70.
- Allen TF. The Encyclopedia of Pure Materia Medica, vol 2. New Delhi;B Jain Publishers ; 1995.
- Hering C. Guiding Symptoms of Our Materia Medica. vol 2. New Delhi:B Jain Publishers; 1995.
- Clarke J H. A Dictionary of Practical Materia Medica.,vol 1.New Delhi :B Jain Publishers;1995.
About the author:
By Dr Anit Singh (Acharya)1*
1.Assistant Professor, Department of Materia Medica,
Dr M P K Homoeopathic Medical College, Saipura, Jaipur.