Effectiveness of Thyroidinum in 3X vis-à-vis 200CH potency in the treatment of hypothyroidism: a prospective, open-label, exploratory trial
Background: The growing prevalence of hypothyroidism emerges as a public health challenge in our society. The therapeutic index of levothyroxine decreases the quality of life, causes long term complications in spite of normal biochemical range. This therapeutic dilemma developed the need to formulate an effective method for reliable prescriptions which would result in a successful outcome for the treatment of hypothyroidism. Homoeopathic medicines Thyroidinum in 3X and 200CH potencies have its probable effects on hypothyroidism, but their comparisons in both potencies have not yet been evaluated systematically. Hence, we aimed to compare the effects of homoeopathic medicine Thyroidinum 3X against 200CH in treatment of hypothyroidism.
Objectives: To assess the effectiveness of different potencies (3X or 200CH) of Thyroidinum at the clinical level by using Zulewski’s clinical score and at biochemical level to determine changes in TSH level.
Methods: A prospective, open label, exploratory trial was conducted at Dr Madan Pratap Khunteta Homoeopathic Medical College, Hospital and Research Institute, Jaipur, Rajasthan, India, from 2015 to 2016. In this study, 100 patients were screened, out of which 70 patients were recruited as meeting the eligibility criteria of the study. With the aid of computer generated random number table participants were allocated to either group A (n=35) or group B (n=35) and received intervention Thyroidinum 3X or 200CH respectively. The outcomes of the study involves the assessments of effects of potency 3X or 200CH of Thyroidinum using the parameter scale Zulewski’s clinical score (ZCS) and assessment of thyroid stimulating hormone (TSH) value and follow-up assessment was done within two weeks or as per requirement or condition of the patient.
Results: Statistical analysis of data was done by applying independent sample t- test and chi-squared statistical tests. On the basis of Zulewski’s clinical score marked difference in score of ZCS (Mean ± SD: 4.06 ± 2.69) in Thyroidinum 3X as compared to Thyroidinum 200CH (Mean ± SD: 2.49 ± 1.25) and P-value is <0.05 after treatment indicating significant difference. Also, changes have been observed in TSH value, treatment under Thyroidinum 3X showed marked difference in score of TSH than Thyroidinum 200CH.
Conclusion: The present study shows the significant improvement in clinical and biochemical (TSH) level in the cases of hypothyroidism using the medicine Thyroidinum 3X as compared to Thyroidinum 200CH. Also, add the treatment efficacy and validate the symptomatology of sarcode, i.e. Thyroidinum on the basis of successful prescriptions and outcome. In future, more rigorous studies can be planned to validate this evidence.
Keywords: Hypothyroidism, TSH, Thyroidinum 3X, Thyroidinum 200CH, Zulewski’s clinical score (ZCS).
Abbreviations: Zulewski’s clinical score (ZCS), free thyroxine (FT4), thyroid stimulating hormone (TSH), thyroid peroxidase antibody (TPO)
Introduction
In current scenario hypothyroidism results from abnormality present in the thyroid gland itself [1] reflecting inadequate production of thyroid hormone or suboptimal action of thyroid hormone on the target tissue,[2] indicates reduction in FT4 and increase in serum TSH.[3] In India, the prevalence of hypothyroidism is around 10.95%.[4] Hypothyroidism is 08–09 times more common in women than in men, and the prevalence increases with age, with a peak incidence between the ages of 30 and 50 years.[5] Hypothyroidism may be clinical (overt hypothyroidism) and mild or subclinical hypothyroidism.[6] These include clinical signs and symptoms such as fatigue, weight gain, constipation, cold intolerance, menstrual irregularities, diffuse muscle pain, hair thinning or loss, dry skin, poor concentration, depression and proximal muscle weakness.[7] The conventional line of treatment present is administration of levothyroxine (LT4).[8] The lifestyle impact and stress can upset optimal thyroid function and apart from this, nutrition play critical role in thyroid hormone synthesis.[9] Despite achieving biochemical euthyroidism with the advancement in the field of therapy for hypothyroidism, various studies [10] [11] have shown inadequate therapeutic surveillance resulting in poor outcome of treatment in terms of presence of residual symptoms compounded with patient dissatisfaction, poor compliance, poorer quality of life with side effects such as impairment in psychological wellbeing, decrease bone mineral density, atrial fibrillation, changes in left ventricular functionand unfeasibility in cost effective. [12]
A case report of 16-year-old female patient highlights role of homoeopathic medicines when prescribed on the basis of totality of symptoms where Ignatia amara followed by Natrum muraticum in subsequent potencies helps in reversing the functional disturbance of thyroid gland evidenced by obtaining improvement in serial thyroid function test (TFT) and Zulewski’s clinical score.[7] A case series, three cases were presented with symptoms of hypothyroidism, constitutional homoeopathic medicines – Calcarea carbonica 200, Pulsatilla nigricans 200, Sulphur 200 were prescribed and followed for a period of 03 months. The reduction obtained in the level of TSH along with improvement in clinical symptoms before and after treatment this favors the response of homoeopathic treatment in the cases of hypothyroidism. [13]
Manchanda et al, conducted an exploratory, randomised, placebo controlled, single blind trial was conducted on 194 school children suffering from subclinical hypothyroidism with or without autoimmune thyroiditis indicates that after post treatment in verum subgroups (group A and C) TSH reached within normal limits in 85.94 and 64.29% in control subgroups and in (group A and B) serum anti TPO titre reached within normal limits in 70.27% and 27.02% in controls. In control group eight children (10.5%) fall under overt hypothyroidism. [14]
The domain of literature review contains existing evidence from case report; case series to randomised controlled trial indicates the positive role of individualised homoeopathic interventions in cases of hypothyroidism including subclinical hypothyroidism. Apart from individualised or constitutional treatment, as per the Paracelsus principle, organopathic therapeutic application [15] assumes that certain remedies have a specific affinity for certain organs; and it is necessary to treat specific organ or system in order to maintain harmony of the whole person.[16] To address these knowledge gaps, the present study an open-label, randomized, exploratory trial was undertaken as with the increasing reliance on alternative treatment, there is need to formulate methods for the effective and reliable prescriptions. Homoeopathy offers a wide range of medicines for the treatment of hypothyroidism. Apart from this, Thyroidinum is used frequently by homoeopathic practitioners, alone or with other medicines for the treatment of hypothyroidism in all age groups. The existing shreds of evidence are limited in relation to effects, potency and dosage which should be proved beneficial in the cases of hypothyroidism. The objective of the study to assess the effectiveness of different potencies (3X or 200CH) of Thyroidinum at the clinical level by using scale Zulewski’s clinical score and at biochemical level to determine changes in TSH level.
Materials and methods
Study design
This is a prospective, open-label, exploratory study.
Study setup
This study was conducted at the Dr. Madan Pratap Khunteta Homoeopathic Medical College, Hospital and Research Centre – Sindhi camp and Saipura campus, Sanganer, Jaipur.
Study duration
The study was under taken for a period of one year of duration, from August 2015 to August 2016, cases were registered in first nine months up to May 2016 and minimum six visits/ observations was obtained for each case.
Inclusion/ exclusion
Participants of age group between 15 years to 40 years, irrespective of their sex, caste, religion and duration of illness were the diagnosed of hypothyroidism (ICD 10 code E03.9) taking treatment from other systems of medicine, feeling no relief and seeking homoeopathic treatment, and also visited for complaints of fatigue, feeling heaviness in whole body, constipation, muscle stiffness, dry skin, and menorrhagia with confirmed by laboratory investigations for hypothyroidism. TSH range included in this study is < 20 mU/L as well as willing to take homoeopathic therapy and ready to hold on allopathic treatment and willing to participate in the study by giving written informed consent. The patients suffering from hypothyroidism secondary to pituitary/hypothalamic diseases, radioiodine ablation, surgery, neck irradiation, patients who were too unwell to take part, inability to read patient information sheets and/or denied consent to take part, pediatric patients <15 years of age, patients with transient hypothyroidism and > 40 years, any severe systemic complications related to hypothyroidism or with other systemic disorders and complications affecting quality of life, active pregnant women or planning a pregnancy were excluded from the study. Patient pursuing other treatment and were not willing to leave it.
Sample size
The sample size for the study was 100 cases which was screened at baseline characteristics, at power (1-β) =80, α=0.05 and treatment effect d= 0.06 (60%). Of these, 70 were included in the study.
Wash-out period
Patients who were taking medicines previously were kept without medication for some time (depending upon the half-life of the medication they were taking).
Randomisation
In this trial, simple randomisation technique was used with the aid of computer-generated table of random numbers [17] and then numbers were written on pieces of paper and kept into envelopes which were then sealed. The participants were enrolled as per inclusion criteria of the protocol and allocated an even number were assigned to the Group A and given intervention (Thyroidinum 3X) while those received odd numbers were assigned to the Group B and given intervention (Thyroidinum 200CH).
The investigator and the patients both were aware of the generated allocations codes all through the study. An allocated code was maintained till the end of the study. This open list of random numbers with allocated codes was also made available with the pharmacist, and he was instructed for dispensing of either Thyroidinum 3X or Thyroidinum 200CH to the patients according to the chart.
Intervention
Group A patients were given Thyroidinum 3X in the form of tablets (dosage – 4 tablets twice daily for fourteen days) [18] [19] and Group B patients were given Thyroidinum 200CH (dosage- one dose followed by Placebo 30 for fourteen days) in the form of globules. [19] Repetition of medicine was done according to the individual requirement of the cases and by appropriate judgment by the investigator. The medicine was procured from a good manufacturing practice (GMP) certified firm SBL Pvt. Ltd, India. The medicine was directed to be taken orally on clean tongue with empty stomach. The participants were assessed within two weeks for follow up for symptomatic relieve.
Data collection
A detailed case taking form was designed and approved for the study in which the case history of the patients were documented and were kept confidential. These records were used for follow-ups and analysis of the case. Each case had a parameter scale – Zulewski’s clinical score, which is comprised of 7 domains under symptoms and 5 domains under physical signs which were assessed at/baseline and after post treatment of 06 months of duration. [20] To assess biochemical changes, TSH level is also recorded at baseline visit and at the end of the study.
Zulewski’s et al reevaluated the classical signs and symptoms of hypothyroidism in the light of modern laboratory tests, based on signs and symptoms originally chosen by Billewicz and a scoring range was determined in patients with untreated overt hypothyroidism and compared to patients with normal thyroid function. Scores were based on the presence (1) or absence (0) of hypothyroid signs and symptoms. The diagnostic range for this clinical score was established as ≤ 2 = euthyroid; 3–5 = intermediate; >5 = overt hypothyroid. [7]
Outcome assessment
The main outcomes patients were measured by Zulewski’s clinical score scale and changes in serum thyroid stimulating hormone (TSH) at baseline and after 06 months treatment. The improvement indices were made on the basis of marked improvement = score% is > 70%, moderate improvement = score % is 40 to < 70%, mild Improvement = score % is < 40% and Status quo = score 0%.
Statistical analysis
Both descriptive and inferential statistics were applied. Statistical analysis of data was done by statistical package for social sciences (SPSS) (Chicago, Illinois, USA) version 21.0 software after tabulation into Microsoft excel. Independent sample t – test was used to compare between intra groups and chi-squared statistical tests was used for baseline comparability of the groups to assess an association between categorical variables. Categorical variables are expressed as frequencies and percentages. P values were set at less than 0.05 as statistically significant.
Result
In this study, 100 patients were screened, 30 patients were excluded in which 11 patients were not willing to discontinue levothyroxine, 06 patients not willing to participate and denied consent for the study, 09 patients having other systemic disorder as well as complications and remaining 04 patients diagnosed as psychiatric illness and pregnancy. Out of these, as per inclusion criteria, 70 patients enrolled, fulfilling the eligibility criteria, and further randomised. During one year duration of study availing intervention, 5 patients dropped out, as it was seen that these patient did not turn up for the complete follow-up visit and study population comprised of 70 patients (55 females and 15 males) were completed the trial of the study. (Figure 1)
Baseline characteristics
The Group A (Thyroidinum 3X) and Group B (Thyroidinum 200CH) participants were comparable as per baseline characteristics, no significant baseline differences existed between groups in terms of socio-demographic characteristics and symptoms distribution. The distribution of the outcome measures at baseline was also similar between the two groups with no significant difference (P>0.01). It implied that both groups were comparable at baseline. [Table 1]
Table – 2 summarizes findings of Group A (Thyroidinum 3X) and Group B (Thyroidinum 200CH), for the sum of signs and symptoms assessed on the basis of Zulewski’s clinical score demonstrated that ZCS score of Thyroidinum 3X at baseline was 7.14 ± 2.14 (Mean ± SD) and in Thyroidinum 200CH was 7.06 ± 1.81(Mean ± SD) with mean difference was -0.09, P = 0.857 and after 6 follow-ups i.e. after treatment ZCS score in Thyroidinum 3X was 3.09 ± 1.72 (Mean ± SD) and in Thyroidinum 200CH score was 4.57 ± 1.93 (Mean ± SD), P = 0.001, with difference score of ZCS in Thyroidinum 3X was 4.06 ± 2.69 (Mean ± SD) and in Thyroidinum 200CH, difference score of ZCS was 2.49 ± 1.25 (Mean ± SD).
As shown in Table – 3, Group A and Group B with assigned intervention of Thyroidinum 3X and Thyroidinum 200CH when assessed according to the TSH, at base line the TSH value was 10.41±3.48 (Mean ± SD) and 9.72 ± 3.33 (Mean ± SD) with mean difference was -0.69, P – value was 0.398 and at end point of study, treatment score was 4.85 ± 1.44 (Mean ± SD) in Thyroidinum 3X and in Thyroidinum 200C TSH value was 6.19 ± 3.35, P-value 0.033, with difference score of TSH was 5.56 ± 2.61 (Mean ± SD) and 3.53 ± 3.21(Mean ± SD).
As depicted in figure 2: The outcome assessment was done with Zulewski’s clinical score on the basis of score % obtained after the response treatment under interventions used Thyroidinum 3X and Thyroidinum 200CH in Group A and Group B. In Thyroidinum 3X, out of 35 cases, 19 cases (54.28%) showed marked improvement in their signs and symptoms attained score% > 70%,14 cases (40%) showed moderate improvement attained score% between 40 to 70%, 20 cases (57.14%) showed mild improvement attained score% <40%, whereas 2 cases (6%) were status quo and depicted no improvement in the symptoms. In Thyroidinum 200CH, out of 35 cases, 2 cases (6%) showed marked improvement in their signs and symptoms attained score% > 70%,5 cases (14.28%) showed moderate improvement attained score% between 40 to 70%, 9 cases (26%) showed mild improvement attained score% <40%, whereas 4 cases (11.42%) were status quo and depicted no improvement in the symptoms.
Discussion
In the current scenario, as the advances in the field of technology, large number of patients is being detected with hypothyroidism [21] and even after proper line of treatment with normal TSH value, results in unsympathetic dismissal of symptoms attributed to hypothyroidism. Therefore, this clinical situation often poses a therapeutic dilemma. [22]
In the study population, a significantly higher proportion of females (79%) were diagnosed with hypothyroidism than male (21%) to draw attention to the growing health needs of this important segment of the Indian population and this findings are similar with a hospital based study from South-India (Hyderabad) shows the prevalence of hypothyroidism was highest in the females 33.52% (n=516) as compared to males were 2.32%. [23] It seems that this gender difference raised as thyroid disorder is by nature autoimmune [24] and immune reactivity is greater in females than in males. [25] The prevalence of hypothyroidism increases with age, as it shown in cross – sectional, multi-centered epidemiology study conducted at eight cities in India[4] it was found that older adults had greater chances of being diagnosed of hypothyroidism with an average age of 31-40 years, i.e. 57.14% as compared to young adults aged 15-30 years i.e. 43% and 21.42% were in the age group 26-30 years was found, he age-group of 46 to 54 years (13.11%,n= 5376) shown the highest prevalence of hypothyroidism as compared to 18 to 35 years of age group in above said study(4) (7.53%).[4]
The manifestations of hypothyroidism in terms of clinical sign and symptoms include a wide variety and often non-specific and may be asymptomatic that differ with age, sex, onset, duration and severity of thyroid hormone deficiency. [26] In this study, the most frequently reported clinical features of hypothyroidism were gastrointestinal symptoms (constipation/flatulence) (87.14%) followed by fatigue (83%), followed by most common sign was puffiness in (71.42%), approximately (69%) study female’s experienced menstrual dysfunction that were not attained menopause with commonest complaint of oligomenorrhoea founded in 30% females. Frequency of headache was 67.14% in this study which is consistent with a prospective study done on headache in hypothyroidism and it was observed that the frequency of headache was (30%, n=102), cold intolerance (57.14%) and perspiration (56%). [27]
In this study, 26 patients (37.14%) had positive family history of hypothyroidism which is in line with a clinical study done on 30 cases of subclinical hypothyroidism where 16% cases had a family history of hypothyroidism. [28] From the conducted experiment, it is observed that, overall result of study population according to statistical analysis, Group A and Group B received intervention Thyroidinum 3X and Thyroidinum 200CH when assessed on the basis of Zulewski’s score depicted marked difference in score of ZCS (Mean ± SD; 4.06 ± 2.69) in Thyroidinum 3X as compared to Thyroidinum 200CH (Mean ± SD; 2.49 ± 1.25) and P-value is less than 0.05 after treatment indicating significant difference. Moreover when assessed on the basis of TSH value, it was observed that after treatment under Thyroidinum 3X marked difference in score of TSH than Thyroidinum 200CH. This study findings parallel to study done on 40 patients on outcome of treating hypothyroidism with Thyroideum (dried thyroid gland) reported an increased in daily doses to 2 tablets (0.4mg of iodine) produced nearly complete compensation of hypothyreosis.[29]
In this study it was observed that when Thyroidinum 3X was prescribed in 35 cases not even a single case of acute, sub-acute and chronic toxicity was reported even in that 6% of cases where Thyroidinum 3X not acted which is consistent with literature. A collaborative study done by All India Institute of Medical sciences and Central Council for Research in Homoeopathy, Government of India, New Delhi, on safety studies of homoeopathic drugs (Ferrum phosphoricum 3X, Ferrum phosphoricum 6X, Calcarea phosphoricum 6X, and Magnesium phosphoricum 6X) in acute, sub-acute and chronic toxicity in rats and on the basis of biochemical, hematological parameters and histopathology of heart, kidney, liver, brain, ovaries and testis was tested and it was found that no adverse effected was reported even after administering for 180 days.[30]
This study focus on the following symptomatology covered by the maximum patients enrolled which is similar with the symptomatology of Thyroidinum. (Table – 4) Clarke mention in his lecture that in cases where thyroid gland is absent or defective, thyroid feeding is to be done to compensate physiological want. [31]
This study identified the most useful potency i.e. Thyroidinum 3X as compared to Thyroidinum 200CH which warranted treatment as a fast and viable solution in the domain of homoeopathic armentarium. The findings indicated that homoeopathic medical therapy might play a beneficial role in the long-term care of patients with such endocrine disorder. This study outcome upgrades the domain of materia medica literature in line with validation of symptoms of the pre-identified drug, Sarcode Thyroidinum with focused on symptomatology (generals and particulars) commonly observed in the patients suffering from hypothyroidism. This approach expands the treatment purpose easier in clinical practice by drawing meaningful symptomatic data.
This study achieved the aimed towards betterment of the patients who is affected from hypothyroidism by using scale (ZCS) and biochemical parameter (TSH) which helps in evaluating the effects of Thyroidinum. The different approaches towards potency covered and improve the knowledge of clinicians and researchers and helping the physicians in their daily practice which is required as with the increasing reliance on alternative treatment. So this study result fuel the existing literature of materia medica on Thyroidinum and also create bridge in the field of organon of medicine in relation to potency, dose and repetition schedule. This study highlighted that Thyroidinum 3X was not shown any toxicity when frequently prescribed is a positive finding of the study.
Limitations of this study include the sample size was inadequate and the time period for the study was of short duration and in addition unable to assess the role of Thyroidinum 3X and 200CH in controlling recurrence of disease after reaching at normalization on the basis of symptomatology and biochemical parameters. In the absence of control arm, there is always a chance of overestimation of the treatment effect. During the study period, as per condition of the patient if any required higher potency or change of potency is limited as to follow the protocol of the study. This is exploratory trial, so therapeutic approach of Thyroidinum is very limited yet. However, as such, is not generalizable to the community.
Benefit to the mankind
According to American thyroid association, in conventional mode of treatment, it is seen that there is no cure for hypothyroidism and have to take lifelong treatment of thyroxine and should never be stopped otherwise health condition may get worse. [32]The findings of this research lead a potential role of Thyroidinum 3X in the treatment of hypothyroidism and reduce the dependence on synthetic thyroxine throughout life. In addition, also help suffering fraternity in managing residual symptoms of hypothyroidism, preventing complications and progression to overt hypothyroidism and also help in combating poor quality of life by shortening the duration of suffering with ease on mental stress regarding the suffering. This positive approach may also provide medical benefits to large population with respect to healthcare cost.
Future strategy
This study supposed to open the pathway for further studies on the 200CH potency of Thyroidinum to explore the data and it should be compared further with higher potencies along with this further studies should be done on dosage and repetition schedule of Thyroidinum 3X and Thyroidinum 200CH. Studies with bigger sample size and longer follow-ups are necessary to provide better and valid result to establish in the general population for the treatment purpose. The clinical trials should be conducted to verify the proving data and pathogenesis of Sarcode Thyroidinum which is mentioned in available homoeopathic literature. To verify the effects of treatment, the need of rigorous methodology of trial explorations such as randomized control trials/comparative cohort should be warranted along with blinding techniques should be included. In order to consolidate the findings observed in the pilot study, a multi centric study on larger scale shall be undertaken to ascertain true effects. Some distinct comparison groups are required to assess whether treatment results vary with individualized medicines selected on the basis of totality of symptoms or with specific medicines for a clinical condition and moreover therapeutic and biological effect of such Sarcode should be undertaken to explore the scope in widest range. So, that it can provide advantage into clinical practice
Conclusion:
The conclusion proposing of this study, based on Zulewski’s clinical score scale and TSH score after post treatment determined statistically significant improvement with Thyroidinum 3X as compared to Thyroidinum 200CH in the management of cases of hypothyroidism. Moreover, this study may help to frame a strategic plan for treatment of such cases.
Acknowledgment:
With a profound sense of gratitude, the author expresses their sincere respect to patient who actively participated in this study and for keeping patience throughout the follow-ups.
Conflict of interest:
The authors declare that they have no competing interest.
Financial support and sponsorship: Nil.
Author’s contributions:
Dr Anuradha Singh – Concept and study design, literature search, data extraction and interpretation, and preparation of manuscript.
Dr Hanuman Ram – Data extraction and interpretation, and preparation of manuscript.
Dr Prasoon Choudhary – Study administration and Supervision
Arvind Kumar – Data extraction and interpretation
Dr Ramesh Prasad – Data interpretation and manuscript review.
References
1. Khandelwal D, Tandon N. Overt and Sub clinical Hypothyroidism: who to treat and how.
Drugs. Jan 2012, 72(1):17-33.
2. Patil AD. Link between hypothyroidism and small intestinal bacterial overgrowth. Indian
Journal of Endocrinology and Metabolism. 2014, 18(3):307-309.
3. Kostoglou AI, Ntalles K. Hypothyroidism- new aspects of an old disease. Hippokratia.
April 2010, 14(2):82-87.
4. Unnikrishnan AG, Kalra S, Sahay RK, Bantwal G, John M, Tewari N. Prevalence of
Hypothyroidism in adults: An epidemiological study in eight cities of India. Indian
Journal of Endocrinology and Metabolism. 2013, 17(4):647-52.
5. Chiovato L, Magri F, Carle A. Hypothyroidism in Context: Where We’ve Been and
Where We’re Going. Advances in Therapy. 2019, 36 (Suppl 2):47-58.
6. De Carvalho GA, Paz-Filho G, Junior CM, Graf H. Management of Endocrine Disease:
Pitfalls on the replacement therapy for primary and central hypothyroidism in adults. Euopean
Journal of endocrinology. 2018, 178(6): R231-244.
7. Singh A, Ram H, Bagdi N, Choudhary P. Management of Primary Hypothyroidism through
Homoeopathy Medicine: A Case Report. World Journal of Pharmaceutical Research. 9(6):
1559-1574.
8. Jonklaas J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, Celi FS, Cooper DS, Kim
BW, Peeters RP, Rosenthal MS, Sawka AM. Guidelines for the treatment of hypothyroidism:
Prepared by the american thyroid association task force on thyroid hormone replacement.
Thyroid. Dec 2014, 24(12):1670-751.
9. Curley PA. Dietary and Lifestyle Interventions to Support Functional Hypothyroidism.
Inquiries Journal/Student Pulse [Online]. 2009, 1(12):1.
10. McAninch EA, Bianco AC. New insights into the variable effects of
Levothyroxine.The Lancet. Diabetes and endocrinology. Oct 2015, 3(10):756-758.
11. Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet. Sept 2017, 390
(10101):1550-1562.
12. Gupta K, Panda NK, Jain P, Bakshi J, Verma R. Hypothyroidism after hemithyroidectomy
for colloid goiter: Is it a reality. Thyroid Research and Practice. Oct 2015, 12(3):107-109.
13. Dogra S, Mandal P. Response of Hypothyroidism to Homoeopathic Treatment: A Report of
Three Cases. Innovare J Med Sci [Internet]. Sep-Oct 2020, 8(5):1.
14. Chauhan VK, Manchanda RK, Narangs A, Marwaha RK, Arora S, Nagpal L, et al. Efficacy
of homoeopathic intervention in subclinical hypothyroidism with or without autoimmune
thyroidistis in children: An exploratory randomized control study. Homoeopathy. 2014, 103
(4):224-231.
15. ChitkaraHL.PrinciplesofPrescribing.NationalHealthPortal.Dec2015.Availablefrom: https://
www.nhp.gov.in/principles-of-prescribing–mtl. Dec 2015. [Last accessed on 2021 April 11].
16. Organ Remedies. Available from: https://www.owenhomoeopathics.com.au/wp-content
/uploads/2016/10/OrganRemedies.pdf. [Last accessed on 2021 April 11].
17. Suresh KP. An overview of randomization techniques: An unbiased assessment of outcome
in clinical research. Journal of human reproductive sciences. 2011, 4(1):8-11.
18. Blackwood AL.A Manual of Materia Medica, Therapeutics and Pharmacology with Clinical
Index. First Indian Edition. Economic Homoeo Pharmacy, 1959.
19. Mathur KN. Systematic Materia Medica of Homoeopathic Remedies. New Delhi; B. Jain
Publishers (P) Ltd. P-991-997.
20. Kalra S, Khandelwal SK, Goyal A. Clinical scoring scales in thyroidology: A compendium.
Indian Journal of Endocrinology and Metabolism. 2011, 15 (Suppl 2): S 89-94.
21. Unnikrishnan AG, Menon UV. Thyroid disorders in India: An epidemiological
perspective.Indian Journal of Endocrinology and Metabolism. 2011, 15 (6):78-81.
22. Kalra S, Khandelwal SK. Why are our hypothyroid patients unhappy? Is tissue
Hypothyroidism the answer? Indian Journal of Endocrinology and Metabolism Jul 2011.
15(Suppl 2): S95-8.
23. Nusrath F, Baderuzzaman, Syyeda A, Parveen N, M Siraj M, et al. Prevalence and at early
age onset of hypo and hyperthyroidism in postiodization era: A hospital based study from
South India. International Journal of Medical Research and Health Sciences.2015, 4(3):490-
495.
24. El-Shafie KT. Clinical presentation of hypothyroidism. Journal of Family Community Med.
Jan 2003, 10(1):55-58.
25. Ahmed SA, Penhale WJ, Talal N. Sex hormones, immune responses, and autoimmune
diseases. Mechanism of sex hormone action. The American Journal of Pathology. Dec
1985, 121(3):531-51.
26. Patel RP, Jain A. Study of anemia in primary hypothyroidism. Thyroid Research and Pract.
2017, 14(1):22-24.
27. Moreau T, Manceau E, Baleydier FG, Dumas R, Giroud M. Headache in hypothyroidism.
Prevalence and outcome under thyroid hormone therapy. Cephalalgia. Dec 1998. 18(10):687-
689.
28. Panicker V. Genetics of thyroid function and disease. The Clinical Biochemist Reviews. Nov
2011, 32(4): 165-175.
29. Kosowicz J, Sikorska HW, Lacka K. Outcome of treating hypothyroidism with thyreoideum.
Pol Tyg Lek. July 1993, 48(27-28):599-602.
30. Singh S, Kalra P, Karwasra R, Khurana A, Manchanda RK, Gupta YK. Safety studies of
homoeopathic drugs in acute, sub-acute and chronic toxicity in rats. Indian Journal of
Research in Homoeopathy. 2016, 11(1).
31. Clarke J.H. A Dictionary of Practical Materia Medica. Vol-3, 30th impression, New Delhi;
B. Jain Publishers. p1437-1443.
32. Hypothyroidism. American Thyroid Association (ATA). Available from: www.thyroid.org.
file:///C:/Users/acer/AppData/Local/Temp/Hypothyroidism-web-bookletpdf.
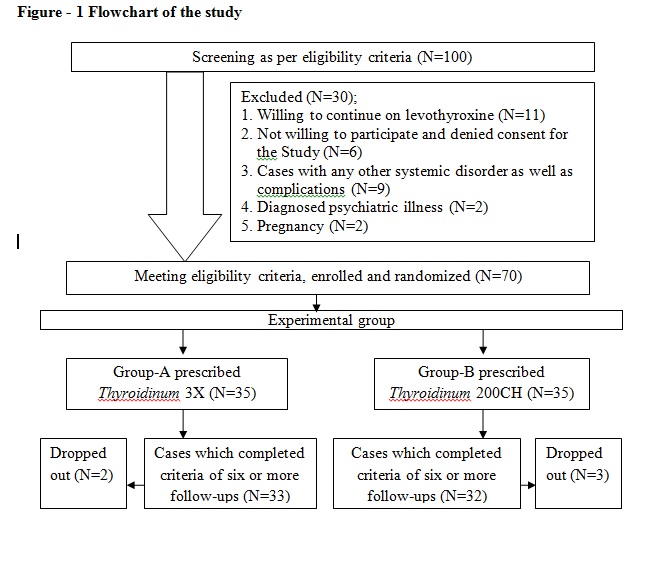
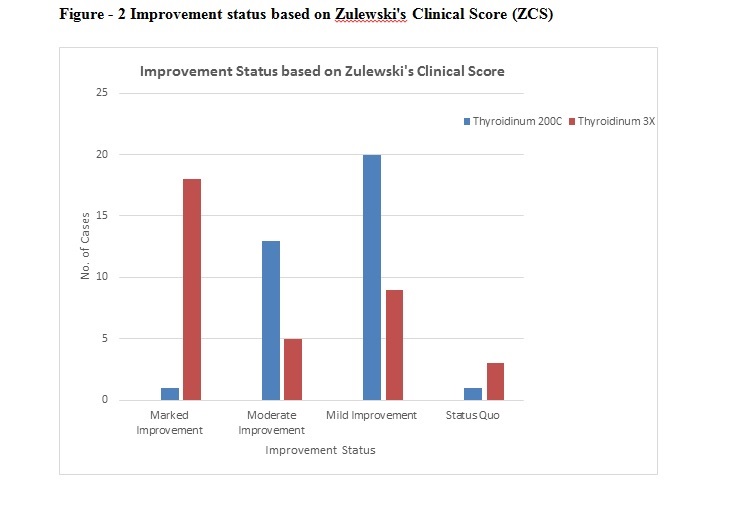
Table – 1: Baseline Characteristics
| Variables | Thyroidinum 3X n=35 (%) | Thyroidinum 200C n=35 (%) | P –value |
| Gender | |||
| Male | 7(20.0%) | 8 (22.9%) | 0.77 |
| Female | 28 (80.0%) | 27 (77.1%) | |
| Age | |||
| Age (years)(M ± SD) | 29.63±7.65 | 32.26±6.77 | 0.133* |
| 15 – 20 Years | 6 (17.1%) | 3 (8.6%) | 0.55 |
| 21 – 25 Years | 3 (8.6%) | 3 (8.6%) | |
| 26 – 30 Years | 8 (22.9%) | 7 (20.0%) | |
| 31 – 35 Years | 11 (31.4%) | 9 (25.7%) | |
| 36 – 40 Years | 7 (20.0%) | 13 (37.1%) | |
| Fatigue | |||
| Absent. | 5 (14.3%) | 7 (20.0%) | 0.53 |
| Present | 30 (85.7%) | 28 (80.0%) | |
| Sweating | |||
| Profuse | 9 (25.7%) | 8 (22.9%) | 0.95 |
| Scanty | 11 (31.4%) | 11 (31.4%) | |
| Normal | 15 (42.9%) | 16 (45.7%) | |
| Constipation/Flatulence | |||
| Constipation | 20 (57.1%) | 21 (60.0%) | 0.54 |
| Flatulence | 9 (25.7%) | 11 (31.4%) | |
| Not Significant | 6 (17.1%) | 3 (8.6%) | |
| Menstrual Complaints | |||
| Oligomenorrhoea | 8 (22.9%) | 13 (37.1%) | 0.23 |
| Menorrhagia | 13 (37.1%) | 6 (17.1%) | |
| Metrorrhagia | 5 (14.3%) | 3 (8.6%) | |
| Not Significant | 2 (5.7%) | 5 (14.3%) | |
| Not applicable | 7 (20.0%) | 8 (22.9%) | |
| Thermal Reaction | |||
| Ambithermal | 5 (14.3%) | 6 (17.1%) | 0.93 |
| Chilly | 20 (57.1%) | 20(57.1%) | |
| Hot | 10 (28.6%) | 9 (25.7%) | |
| Headache | |||
| Absent | 14 (40.0%) | 9 (25.7%) | 0.20 |
| Present | 21 (60.0%) | 26 (74.3%) | |
| Family History of Hypothyroidism | |||
| Absent | 24 (68.6%) | 20 (57.1%) | 0.32 |
| Present | 11 (31.4%) | 15 (42.9%) | |
| Puffiness Location | |||
| Ankle | 10 (28.6%) | 6 (17.1%) | 0.65 |
| Facial | 8 (22.9%) | 8 (22.9%) | |
| Periorbital | 3 (8.6%) | 5 (14.3%) | |
| Not Significant | 14 (40.0%) | 16 (45.7%) |
Table – 2 Zulewski’s clinical score (ZCS)
| Zulewski’s Clinical Score (ZCS) | Thyroidinum 3X (n=35) (Mean ±SD) | Thyroidinum 200CH (n=35) (Mean ±SD) | Mean Difference | 95% Confidence Interval of the Difference | P-value* |
| Before treatment Score | 7.14±2.14 | 7.06±1.81 | -0.09 | (-1.03 to 0.86) | 0.857 |
| After treatment Score | 3.09±1.72 | 4.57±1.93 | 1.49 | (0.61 to2.36) | 0.001 |
| Difference Score of ZCS | 4.06±2.69 | 2.49±1.25 | -1.57 | (-2.57 to -0.57) | 0.003 |
| Score % | 53.30±26.71 | 36.73±18.08 | -16.57 | (-27.45 to -5.69) | 0.003 |
Note: Independent sample t- test *
Table – 3 Thyroid stimulating hormone (TSH) score
| TSH | Thyroidinum 3X (n=35) (Mean ±SD) | Thyroidinum 200CH (n=35) (Mean ±SD) | Mean Difference | 95% Confidence Interval of the Difference | P-value* |
| Before treatment Score | 10.41±3.48 | 9.72±3.33 | -0.69 | (-2.32 to 0.93) | 0.398 |
| After treatment Score | 4.85±1.44 | 6.19±3.35 | 1.34 | (0.11 to 2.57) | 0.033 |
| Difference Score of TSH | 5.56±2.61 | 3.53±3.21 | -2.03 | (-3.36 to -0.71) | 0.003 |
| Score % | 52.45±6.89 | 35.19±26.70 | -17.26 | (-26.56 to -7.95) | 0.00001 |
Note: Independent sample t- test *
Table – 4 Common symptoms found and matched with drug symptoms of Thyroidinum
| Symptoms | Modalities and associations |
| Headache | Dull aching, stitching, pricking, bursting and throbbing. Aggravation – Strong odours, open air, thinking, sun exposure, night, morning, bending forward. Amelioration – tight bandaging, rest, lying down |
| Constipation | Painful, dry, hard, difficulty in passing stool, unsatisfactory and urge to pass stool |
| Flatulence, Sour eructation, Regurgitation of food | Painful, fullness, heaviness in head Aggravation – before and after eating, raw onion |
| Perspiration profuse | Face, axillae, palm and sloe |
| Oedema | Face, peri orbital region, arms, legs and ankle joint |
| Physical fatigue | Present |
| Menstrual irregularities (early, delayed, inter-menstrual bleeding) | Flow – profuse, scanty, clotted blood, offensive |
About Author:
1Dr Anuradha Singh, 2Dr Hanuman Ram, 3Dr Prasoon Choudhary, 4Dr Ramesh Prasad,
5Arvind Kumar
1Senior Research Fellow (H), Central Research Institute, Pratap Nagar, Jaipur, Rajasthan. Formerly PGT in Dept. of Homoeopathic Materia Medica, Dr M.P.K. Homoeopathic Medical College, Hospital and Research Institute, Jaipur, Rajasthan. Pin code – 302033.
2Assistant Professor, Dept. of Homoeopathic Materia Medica, Madhav Homoeopathic Medical College and Hospital, Abu Road, Sirohi, Rajasthan. Pin code – 307026.
3HOD and Professor, Dept. of Pediatrics, Dr M.P.K. Homoeopathic Medical College, Hospital and Research Institute, Jaipur, Rajasthan. Pin code – 302027.
4Research Officer (H), S-3, CTU Homoeopathy on (Viral Encephalitis), B.R.D. Medical College and Hospital Gorakhpur, UP. Pin code- 273013
5Statistical Assistant, Central Council for Research in Homoeopathy (HQ), Janakpuri D block, New Delhi. Pin code – 110058.
Corresponding author –
Dr Hanuman Ram, Assistant Professor, Dept. of Homoeopathic Materia Medica, Madhav Homoeopathic Medical College and Hospital, Abu Road, Sirohi, Rajasthan.