A Case of Scalp Psoriasis And Individualistic Homoeopathic Treatment
Abstract :
Psoriasis is a common, chronic, inflammatory, multisystem disease with predominantly skin and joint manifestations affecting approximately 2% of the population. In this fourth of 6 sections of the guidelines of care for psoriasis, we discuss the use of traditional systemic medications for the treatment of patients with psoriasis. Treatment should be tailored to meet individual patients’ needs. We will discuss in detail the efficacy and safety, and offer recommendations for the use of the 3 most commonly used, and approved, traditional systemic agents: methotrexate, cyclosporine, and acitretin. We will also briefly discuss the available data for the use of azathioprine, fumaric acid esters, hydroxyurea, leflunomide, mycophenolate mofetil, sulfasalazine, tacrolimus, and 6-thioguanine in psoriasis.
Keywords: scalp psoriasis, homoeopathy.
Introduction:
Psoriasis is a chronic inflammatory, hyperproliferative skin disease. It is characterised by well-defined, erythematous scaly plaques, particularly affecting extensor surfaces, scalp and nails, and usually follows a relapsing and remitting course. Psoriasis affects approximately 1.5%-3% of populations of European ancestry but is less common in Asian, South American and African populations. It occurs equally in both sexes and at any age; although it is uncommon under the age of 5 years, more than 50% of patients present before the age of 30 years. The age of onset follows a bimodal distribution, with an early-onset type in the teenage or early adult years, often with a family history of psoriasis, a more severe disease course and strong HLA association. The later-onset type is typically seen between 50 and 60 years, usually without a family history and with a less severe disease course.
Exacerbating Factors In Psoriasis:
Trauma
• Lesions can appear at sites of skin trauma, such as scratches or surgical .
• Wounds ( Köbner isomorphic phenomenon).
Infection
• β-haemolytic streptococcal throat infections often precede Guttate psoriasis . • Severe psoriasis may be the initial presentation of HIV infection.
Sunlight
• Psoriasis may occur or worsen after sun exposure, mainly due to Köbnerisation . • At sites of sunburn or polymorphic light eruption.
Drugs
• Antimalarials, β-adrenoceptor antagonists (β-blockers), lithium, NSAIDs and . • TNF-α inhibitors can exacerbate psoriasis.
• ‘Rebound’ are of psoriasis may occur after withdrawal of systemic .
• Glucocorticoids or potent topical glucocorticoids. Rebound psoriasis is often . • Unstable and may be pustular.
Psychological factors
• Anxiety and stress may exacerbate psoriasis in predisposed individuals.
• HIV = human immunodeficiency virus; NSAIDs = non-steroidal anti-inflammatory drugs; TNF-α = tumour necrosis factor alpha).
Type Different Diagnosis
1.Guttate psoriasis – Maculopapular drug eruption, secondary syphilis pityriasis rosea.
2.Small plaques – seborrhoeic dermatitis; Lichen simplex chronicus (LSC); tinea corporis; cutaneous T-cell lymphoma (CTCI.); Psoriasiform drug eruptions.
3.Large plaques – Dermatophytosis; CTCL.
4.Scalp – Dermatophytosis; Seborrheic dermatitis.
5.Inverse – Intertrigo; dermatophytosis; candidiasis; Extramammary Paget’s Disease (EMPD); Glucagonoma syndrome; Hand-Schüller-Christian disease (histiocytosis), familial Benign pemphigus (Hailey-Hailey disease).
6.Nail involvement – Nail fungal infections.
7.Erythrodermic type – Generalized eczema: CTCL.
8.Generalized pustular psoriasis – Subcorneal pustular dermatosis, Pemphigus foliaceus, Impetigo, Migratory Necrolytic erythema, widespread candidal infection. 9.Localized pustular psoriasis – Infected eczema, fungal infection on the soles.
10.Acral involvement – Herpes simplex, streptococcal and candidal infection.
11.Seborrheic psoriasis – Seborrheic dermatitis.
12.Childhood psoriasis – Dermatitis; candidal infection.
13.Inverse – Seborrheic Dermatitis; Fungal Infections; Erythrasma
Common Signs And Symptoms:
• Common signs and symptoms include:
• Red patches of skin covered with thick, silvery scales
• Small scaling spots (commonly seen in children)
• Dry, cracked skin that may bleed
• Itching, burning or soreness
• Thickened, pitted or ridged nails
• Swollen and stiff joints.
Diagnosis:
• The diagnosis of psoriasis is primarily clinical. There are different clinical types of psoriasis ,1 the most common of which is chronic plaque psoriasis, affecting 80% to 90% of patients with psoriasis.
• The hallmark of classic plaque psoriasis is well-demarcated, symmetric, and erythematous plaques with overlying silvery scale .
• Plaques are typically located on the scalp, trunk, buttocks, and extremities but can occur anywhere on the body. Patients might demonstrate nail involvement, which can present without concomitant plaques.
• Active lesions might be itchy or painful. Psoriasis can also present as an isomorphic response, where new lesions develop on previously normal skin that has sustained trauma or injury. The severity of disease can be helpful in guiding management and is classified as mild, moderate, and severe .
GRATTAGE TEST:
when an attempt is made to scrap the psoriasis plaque, it becomes silvery. On further scraping a thin membrane of skin comes out resulting into multiple pin point bleeding spots. This is known as auspitz sign and the whole process is called a grattage test.
Clinical Evaluation:
For people with any type of psoriasis assess:
• Disease severity
• The impact of disease on physical, psychological and social wellbeing
• Whether they have psoriatic arthritis
• Presence of comorbidities.
Assess the severity and impact of any type of psoriasis:
• At the first presentation.
• Before referral for specialist advice and at each referral point in the treatment. • Pathway to evaluate the usefulness of interventions,
When assessing the disease severity, record:
• Physician’s Global Assessment
• Patient’s assessment of current disease severity.
• Body surface area (BSA) affected
• Any involvement of nails, high-impact and difficult-to-treat sites (for example, the face, scalp, palms, soles, flexures and genitals)
• Any systemic upset such as fever and malaise.
Investigations:
In cases where there is diagnostic uncertainty, skin biopsy is conducted to confirm the diagnosis of psoriasis.
Case Presentation :
Mrs. A of age 32 came with the complaints of violent itching in scalp Falling of large thick scales while scratching, eruptions covered with white, yellow scales , burning sensation after scratch, bleeding after scratching since 2 years special in spring weather . When the patient thinks about his complaints aggravating the complaints, the patient is irritable, anxious about the future. Always irritable in the morning with religious affection.
History of present complaints
She was under treatment in both allopathic and Ayurvedic systems of medicine but it gave temporary relief after 2 years of suffering when she visited our OPD 17 December 2024.
Family history-
Mother suffered from diabetes, sister suffers from dandruff.
Physical Generals
Her appetite was good and cannot remain empty stomach for prolonged periods with an average thirst of 1 to 1.5 litres of water per day. The patient had a desire for sweets, sour food, acid, and aversion to milk. Bowel habits were regular early mornings without any discomfort . Passed urine 1-5 times per day. Sleep was disturbed.
The thermal reaction of the patient is hot (prefer winter and cannot tolerate heat) . A general feeling of weakness accompanies the patient most of the time.
Local and systemic examination
The tongue was clean and moist. Anemia-abcent , cyanosis- absent, lymph anode – not enlarged, pulse-76/min, B.P-120/80 mmhg.
Diagnosis – It is probably a case of Scalp psoriasis.
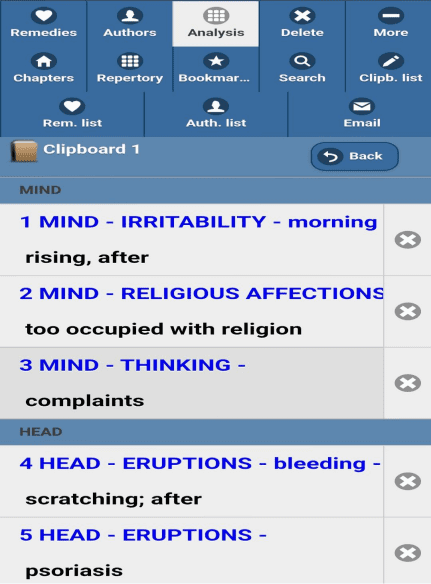
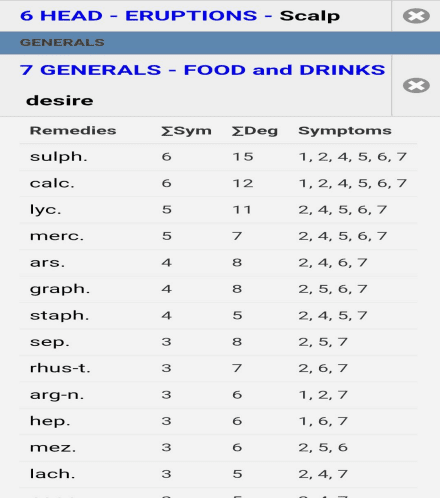
Analysis of case
After analyzing the symptoms of the case the characteristics mental, physical and particular symptoms were considered for framing totality-Morning irritability with religious affection, When the patient thinks about his complaints aggravates the complaints, the patient is irritable, anxiety about future lassitude in general, desire for sour food and acid with early morning diarrhoea were the important general symptoms. Tongue was clean and moist, aversion to milk were included totality. Miasmatic evaluation for the present symptom was done with the help of “The chronic disease by Dr Samuel Hahnemann “ showed the predominance of psoric miasm considering the above mentioned symptoms synthesis repertory was preferred and systemic repetorisation was done. Repetorisation sheet is given below.
Prescription –
Sulphur 1M /single dose
Phytum 500/BD/15day
Reportorial Result:



Follow up –
1st follow up 24/01/25
Symptoms -Patient felt slightly better, itching slightly reduced, burning sensation reduced.
Priscription- Placebo 200 /BD/15 days
2nd follow up 10/02/25
Symptoms -Patient feels better, imitability reduced, itching reduced, falling of scales while scratching reduced, sleep improved.
Priscription- Sulphur 1M/ single dose
Sac- lac 200/BD/15 days
3rd follow up 27/02/25
Symptoms – Patient feels better itching reduced, bleeding after scratching relieved, eruptions covered with white scales slightly reduced.
Prescription- Placebo 200 /BD/15days
4th Follow up 28/03/25
Symptoms -Patient feels better with all complaints, eruptions are getting healed Prescription- Phytum 200 /BD/ 15 day’s
BEFORE:


AFTER:



Conclusion:
Homoeopathy is one of the most popular holistic systems of medicine. The selection of remedy is based upon the theory of individualisation and symptoms similarity by using a holistic approach.
Homoeopathic medicine helps in removing the and triggering factor and reverses skin multiplication back . The patient started homoeopathic medicines and within a month scaling stopped and no new patch appeared. Within 4 months, all the scally patches disappeared, scaling was nil and itching was minimal.
Reference:
1 Mender A, Gottlieb CA, Feldman SR., Voorhees ASV, Leonardi CL Gordon KB, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis. J Am Acad Dermatol Volume 58(3): 826-850.
2.https://www.cimch.edu.bd/assets/files/DavidsonMedicine24th.pdf
3.https://www.researchgate.net/publication/334525145_Introductory_Chapter_Psoriasi s_as_a_Whole.
4. https://pmc.ncbi.nlm.nih.gov/articles/PMC5389757/.
5. https://www.nice.org.uk/guidance/cg153/chapter/Recommendatios. 6. “Synthesis: Repertorium Homoeopathicum Syntheticum”
7.H.C. ALLEN- Allen’s Keynotes
Rearranged and Classified with Leading Remedies of the Materia Medica and Bowel Nosodes including REPERTORIAL INDEX
8. Boericke New manual of Homoeopathic Materia Medica with Repertory. William Boericke, third revised and augmented edition based on ninth edition, B.Jain publishers, New Delhi.pp-82,312,622,588,510,412,555,
9.THE CHRONIC DISEASES,THEIR PECULIAR NATURE AND THEIR HOMEOPATHIC CURE, By DR. SAMUEL HAHNEMANN.Ab
ABOUT THE AUTHORS:
Dr.AARTI MEHTA, B.H.M.S, M.D (Hom), Department of Homoeopathic Materia Medica, Government Homoeopathic Medical College and Hospital Bhopal AYUSH campus, Beside Kaliyasot dam, MACT hills, Bhopal – 462003 (M.P.)
UNDER THE GUIDANCE :
PROF. DR SHOBHANA SHUKLA
Professor and H.O.D. of Department of Homoeopathic Materia Medica, Government Homoeopathic Medical College and Hospital, Bhopal AYUSH campus, beside Kaliyasot dam, MACT hills, Bhopal – 462003 (M.P.) And Ex joint Director .




