Abstract
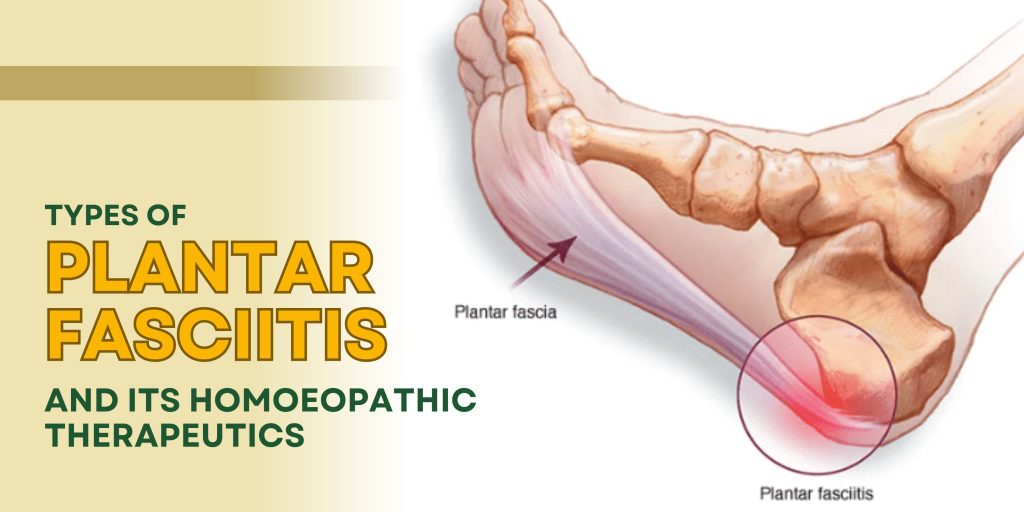
Plantar fasciitis is among the most prevalent causes of inferior heel pain encountered in clinical practice. It is characterized by pain and tenderness at the medial calcaneal tubercle due to inflammation or degeneration of the plantar fascia. Though traditionally considered an inflammatory condition, current understanding indicates that many chronic cases represent a degenerative fasciosis. The condition manifests in various clinical forms depending upon etiology, duration, mechanical strain, metabolic factors, and individual susceptibility. Conventional management focuses on analgesics, physiotherapy, orthotics, corticosteroid injections, and in resistant cases, surgery. Homoeopathy, however, approaches plantar fasciitis from a constitutional and miasmatic perspective, viewing it as an expression of internal imbalance of the vital force. This article provides a comprehensive review of types of plantar fasciitis along with detailed homoeopathic therapeutics based on characteristic symptomatology and individualization.
Keywords
Plantar fasciitis, Heel pain, Homoeopathic therapeutics, Constitutional treatment, Musculoskeletal disorders
INTRODUCTION
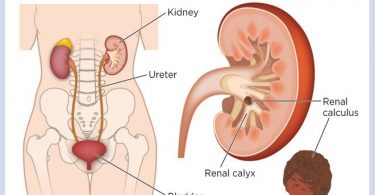
The plantar fascia is a thick fibrous aponeurosis extending from the medial tubercle of the calcaneus to the proximal phalanges. It plays a crucial role in maintaining the medial longitudinal arch of the foot and in absorbing shock during ambulation. Repetitive microtrauma leads to inflammation or degeneration at its origin, producing characteristic heel pain. Epidemiology suggests plantar fasciitis affects approximately 10% of the population at some point in life. It is common in middle-aged individuals, athletes, obese patients, and those engaged in prolonged
standing occupations. Risk factors include obesity, tight Achilles tendon, flat foot, high arches, improper footwear, prolonged standing, diabetes mellitus, and hypothyroidism.
From a homoeopathic perspective, disease is not merely a localized pathology but an outward
manifestation of disturbed vital force. Thus, plantar fasciitis is treated not only locally but constitutionally.
Pathophysiology
Initially, repetitive stress causes microtears in the plantar fascia leading to acute inflammation.
Histopathological studies in chronic cases reveal collagen degeneration, fibroblast proliferation, and myxoid degeneration rather than active inflammatory cell infiltration. This stage is often termed plantar fasciosis.
Biomechanical abnormalities such as excessive pronation increase tensile stress on the fascia.
Obesity increases mechanical load, while systemic disorders impair tissue healing, predisposing to chronicity.
Clinical Features
• Heel pain localized at medial calcaneal tubercle
• Pain worst during first steps in the morning (start-up pain)
• Pain after prolonged rest
• Aggravation by prolonged standing or walking
• Relief after mild activity (in some cases)
• Tenderness on palpation
TYPES OF PLANTAR FASCIITIS
1. Acute Plantar Fasciitis
This type results from sudden overstrain, prolonged walking, or increased physical activity.
Clinical Characteristics:
• Sudden onset sharp heel pain
• Local warmth and tenderness
• Pain aggravated by movement
• Possible redness and swelling
Homoeopathic Therapeutics:
Bryonia alba – Indicated where pain is stitching, worse from slightest motion, better by rest.
There is dryness and irritability.
Rhus toxicodendron – Marked stiffness after rest, pain better from continued motion, worse in cold damp weather.
Belladonna – Sudden inflammatory onset with redness, throbbing pain, and heat.
2. Chronic Plantar Fasciitis
Develops due to persistent strain and degenerative changes.
Clinical Characteristics:
• Long-standing dull aching pain
• Thickening of fascia
• Reduced elasticity
• Pain after prolonged standing
Homoeopathic Therapeutics:
Calcarea carbonica – Suited to obese, flabby individuals with profuse perspiration and cold sensitivity.
Silicea – For weak connective tissue, slow healing, chilly constitution.
Kali carbonicum – Stitching heel pain with marked weakness in lower limbs and back.
3. Mechanical / Overuse-Related Plantar Fasciitis
Seen in athletes, runners, and occupations requiring prolonged standing.
Clinical Characteristics:
• Pain after excessive activity
• Bruised soreness
• Relief with rest
Homoeopathic Therapeutics:
Arnica montana – For trauma and overexertion with bruised feeling.
Ruta graveolens – Acts on tendons and periosteum; pain from overuse.
Calcarea fluorica – Ligamentous strain with loss of elasticity.
4. Degenerative Plantar Fasciitis (Plantar Fasciosis)
Common in elderly individuals where degeneration predominates.
Clinical Characteristics:
• Persistent dull pain
• Minimal inflammatory signs
• Calcaneal spur formation (in some cases)
Homoeopathic Therapeutics:
Symphytum officinale – Deep periosteal pain; promotes tissue repair.
Fluoric acid – Degenerative tissue states, better by cold applications.
Sulphur – Chronic burning pains; constitutional psoric remedy.
5. Plantar Fasciitis Associated with Systemic Conditions
Frequently associated with obesity, diabetes, hypothyroidism.
Clinical Characteristics:
• Poor healing
• Recurrent episodes
• General metabolic imbalance
Homoeopathic Therapeutics:
Natrum muriaticum – Dryness, weakness, reserved emotional state.
Phosphoric acid – Debility from mental strain; exhaustion.
Thuja occidentalis – Chronic constitutional disorders; sycotic background.
Role of Miasmatic Consideration
Psora contributes to functional disturbance and inflammatory tendencies.
Sycosis predisposes to thickening and overgrowth (calcaneal spur).
Syphilis may be associated with destructive degeneration.
Individualization requires evaluation of totality of symptoms including mental, general,
and particular characteristics.
Differential Diagnosis
• Calcaneal spur
• Tarsal tunnel syndrome
• Stress fracture of calcaneus
• Rheumatoid arthritis
• Gout
Investigations
• Clinical diagnosis primarily
• X-ray to detect calcaneal spur
• Ultrasound showing thickened fascia
• MRI in resistant cases
Conventional Management Overview
• Rest and activity modification
• NSAIDs
• Stretching exercises
• Orthotic support
• Steroid injections
• Extracorporeal shockwave therapy
Homoeopathic Management Approach
Case-taking must include:
• Onset and causation
• Modalities (better/worse)
• Thermal state
• Constitution
• Mental and emotional state
• Past history
• Family history
Potency selection depends upon vitality and susceptibility. Acute cases may require
frequent repetition of low or medium potency. Chronic cases often respond to higher potency
with infrequent repetition.
Prognosis
With proper individualization, acute cases respond rapidly. Chronic degenerative cases
require prolonged treatment but show gradual improvement in pain and function.
Discussion
Plantar fasciitis represents a multifactorial condition involving mechanical, metabolic,
and constitutional components. Homoeopathy offers a holistic approach addressing both
local pathology and systemic susceptibility. Proper remedy selection based on symptom
totality improves long-term outcomes and reduces recurrence.
Conclusion
Plantar Fasciitis is not merely a Localized mechanical disorder but reflects deeper
constitutional imbalance. Homoeopathic therapeutics, when prescribed according to
principles of individualization, miasmatic understanding, and totality of symptoms,
can effectively manage various types of plantar fasciitis and prevent recurrence.
References
1. Boericke W. Pocket Manual of Homoeopathic Materia Medica. New Delhi: B. Jain Publishers.
2. Kent JT. Lectures on Homoeopathic Materia Medica. New Delhi: B. Jain Publishers.
3. Hahnemann S. Organon of Medicine. 6th ed. New Delhi: B. Jain Publishers.
4. Clarke JH. Dictionary of Practical Materia Medica. New Delhi: B. Jain Publishers.
5. Buchbinder R. Clinical practice: plantar fasciitis. N Engl J Med. 2004.
6. Riddle DL, Schappert SM. Volume of ambulatory care visits for plantar fasciitis. J Am Podiatr Med Assoc.
7. Wearing SC et al. Plantar fasciitis: are pain and fascial thickness associated, J Orthop Res.
8. Roxas M. Plantar fasciitis: diagnosis and therapeutic considerations.