Dr Yogyata Kashyap
ABSTRACT
Treating skin diseases is quite challenging for the practitioner. If one has the right perception or correct knowledge to reach the diagnosis so that it can become an easy task. For a homoeopath, it is significantly difficult to treat skin disorder without any homoeopathic aid. Through this article, the author has allocated one’s perception and the approach to such kind of patients so as to provide the best homoeopathic treatment.
KEYWORDS- skin lesions, common skin problems, clinical repertories, related rubrics.
ABBREVIATIONS- contact dermatitis (CD) , allergic contact dermatitis(ICD), airborne contact dermatitis(ACD), contact urticaria(CU).
INTRODUCTION
Skin is a visible organ, therefore any blemish, rash or any kind of eruption or diseases on the face or extensive lesions affect the lives as well as mental health. [1] Skin is not only the largest organ but is also an integral component of the body’s defence system. [2] Nowadays occurring of skin diseases is becoming very common. In practice, every second patient come with the complaint of skin problem. People with skin lesions may suffer the effect of stigma, which affect quality of life of patient. So, it becomes necessary to provide best homoeopathic treatment. Before selecting any medicine, the physician’s first aim should be recognising the skin lesions.
- HOW TO DIAGNOSE SKIN LESIONS [1]
- History of skin lesions
- Morphological examination of skin lesions
- History of patient
HISTORY OF SKIN LESIONS
For taking history in a skin disorder patient, one needs to look for two types of symptoms[1]:-
- Subjective symptoms (itching, pain, parenthesis, any other kind of sensation)
- Objective symptoms (rash, any eruption, ulcer, swelling)
A detailed history of these symptoms is necessary-
- SUBJECTIVE SYMPTOMS – further question about subjective symptoms[1].
- Duration
- Site of onset
- Seasonal variation – itching < in winter : ichthyosis
- Diurnal variation – itching- nocturnal < : scabies
- Precipitated by exercise – cholinergic itching
- Associated
features – itching with – rash, wheals
- OBJECTIVE SYMPTOMS – further question about objective symptoms[1].
- Seasonal aggravation – winter: ichthyosis, psoriasis, seborrheic dermatitis.
–Summer/rainy season – fungal infections, bacterial infections, insect bites.
- Site of involvement – extensors, pressure points: psoriasis
scalp, naso-labial folds, flexors: seborrheic dermatitis.
Face, back : acne.
Photo-exposed parts : photosensitive eruption.
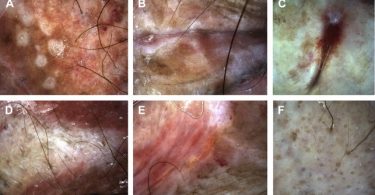
- MORPHOLOGICAL EXAMINATION OF SKIN LESIONS[1][2]
Morphology of the lesions is far more important than their distribution. There are two types of skin lesions – primary lesions and secondary lesions[1].
Primary lesions – Those lesions that are the direct result of a pathologic process[1].
- Macule: Small, flat, non-palpable lesion, no change in skin texture (< 1cm)[1]. For example – freckle.
- Papule: Small solid, elevated, palpable lesions (<1cm)[1]. For example – warts.
- Patch: Large, flat, non-palpable lesion (>1cm). For example[2]: “café-au-lait” spot.
- Plaque: Large, elevated, palpable lesion (>1cm). For example: psoriasis[2].
- Nodule: solid lesion, palpable, some nodule are better felt than seen (<1cm)[1]. For example: enlarged lymph node[2].
- Tumour: Large nodule (>1cm) with deep significant component[2].
- Vesicle: Small, fluid-filled lesion (<1cm)[1]. Example: Blister.
- Bulla: Large, fluid-filled lesion (>1cm)[1].
- Pustule: A pus-filled lesion. Variable sizes[1].
- Abscess: Pus-filled nodule having a thick wall[1].
- Burrow: A thread-like curvilinear papule caused by a burrowing mite[1].
- Comedo: plugged hair follicle. There are two types of comedones- Open comedo(black head) or closed (whitehead)[2].
Secondary lesions – These are the modified lesions of primary lesions by scratching, rubbing, infection, or other events[1].
- Scale: is a flake of keratin that can be fine or corse; loose or adherent. Scales are of different types and may be distinct in some diseases. [1]
Silvery, easily removable – psoriasis
Mica-like, adherent – pityriasis lichenoides chronica
Branny (fine) – pityriasis versicolor
Collarette of scales – pityriasis rosea
- Crust: dried remains of serum, blood or pus overlying involved skin[2].
- Keratosis: horn-like thickening of the skin[1].
- Erosion: erosion results from complete or partial loss of epidermis but no loss of dermis[1].
- Ulcer: is a deep open wound destruction extending into the dermis or may involve subcutaneous tissue[2].
- Fissure: triangular slit in the epidermis[1].
- Sinus: is a channel between two spaces[1].
- Lichenification: Is the result of repeated scratching. Which is characterised by three factors – thickening of skin, hyperpigmentation and increased skin marking[1].
After the identification of primary and secondary lesions has been done, they need to be further classified into:-
- Colour– look for the colour of skin lesions like erythematous, yellow, black, hypopigmentation or hyperpigmentation[1].
- Shape- Lesions can have variety of shapes[1]:
- Nummular(discoid) : nummular dermatitis
- Annular: tinea corporis
- Circinate: herpes simplex
- Arcuate: granuloma annulare
- Gyrate: some forms of tinea
- Retiform (reticulate): macular amyloidosis
- Surface- papules and nodules have variety of shapes[1].
- Dome shaped: molluscum contagiosum
- Flat topped: plane warts
- Umblicated: molluscum contagiosum
- Acuminate: genital warts.
- Verrucous: verruca vulgaris
- Pedunculated: skin tags
- Sharpness of lesions- look for whether the lesions are well defined or ill defined[1].
- Distribution of lesions- distribution is another aspect of the skin lesions which helps a physician to make a diagnosis[1].
- Acne: Face, trunk, deltoid region.
- Photo dermatitis: exposed area of skin like- face, neck, dorsolateral aspect of the forearms, sparing of covered parts
- Seborrhoeic dermatitis: scalp, nasolabial folds, folds, front of the chest, axillae, groins.
- Arrangements: after identifying the lesions primary or secondary, one must identify the arrangement of the lesions[1].
- Grouped: Gathered together. For example, herpes simplex
- Linear: Resembling a straight line. For example, linear epidermal naevus
- Dermatomal: distributed along dermatomal. For example, herpes zoster
- Serpiginous: wavy or curvy like a serpent. For example, burrow
- Arcuate: curved, resembling an arc. For example, granuloma annulare.
- HISTORY OF PATIENT
After completing the history taking about skin lesions, another important part to approach a skin patient is the history of patient. It may sometime assist the physician in reaching a diagnosis. In this part, it includes:-
- Past
history
–we look for- Any past medical, surgical history is important in drug eruption.
Any past infection, history of medical disorder like diabetes, Asthma, hay
fever, eczema, or any other type of allergy should be noted. History of using
any kind of topical application to treating skin problem. Any kind of
self-medication. Drug reaction in past[1].
- Personal
history-
it includes his occupational, social, travel history. There are many such
diseases which are caused by exposure to hazards at work[1].
- Chemical hazards- Irritants, sensitising, photosensitising and acnegenic agents[3].
- Biological hazards- Bacteria, fungi, viri, to skin parasite.
- Physical hazards- Rubbing, radiations, temperature and mechanical pressure[3].
- Personal
history-
it includes his occupational, social, travel history. There are many such
diseases which are caused by exposure to hazards at work[1].
The most common occupational skin disorder is contact dermatitis, other are irritant contact dermatitis(CD) , allergic contact dermatitis(ICD), airborne contact dermatitis(ACD), contact urticaria(CU)[3].
- Family history- especially skin disorder, atopic disorder[1]. Habit- smoking, alcohol, tobacco chewing, drug intake[1].
HOMOEOPATHIC MANAGEMENT OF COMMON SKIN DISORDERS USING CLINICAL REPERTORIES
Phatak Repertory[4]:
ACNE- Hep, Merc
ERUPTIONS, TENDENCY TO- Acon, ARS, CALC, Caust, Clem, Dulc, Graph, Lach, LYC, MERC, Mez, Nat-m, Nit-ac, phos, Puls, RHUS-T, SEP, SIL, SULPH.
ERUPTIONS, TENDENCY TO, ACNE- Hep, Merc
ERUPTIONS, TENDENCY TO , PSORIASIS – Ars-i, Clem, Dulc, Graph, Phos, Ran-b, Sep, Sulph.
ERUPTIONS, TENDENCY TO, PSORIASIS, scales, shining – iris
ERUPTION, TENDENCY TO, itch-like, scabies- Carb-v, Caust, MERC, Sel, Sep, SULPH.
LEUCODERMA- Sil, Sulph.
RINGWORM ALL OVER, THE BODY- psor, ran-b.
URTICARIA, HIVES, WHEALS – Apis, CALC, Caust, Dulc, Hep, RHUS-T, Urt-u.
WARTS, Horny – ant-c, sil.
WARTS, flat.- berb, caust, Dulc, merc-i-f, ruta.
WARTS, pedunculated – Thuj.
Boericke Repertory[5]
FACE, eruptions on face, acne rosacea – ARS-BR, Carb-an, Chrysar, EUG, KREOS, Psor, Sul-ac, Zinc.
FACE, eruptions on face, acne simplex – ANT-C, BELL, BERB-A, EUG, JUG-R, LED, NUX-V, SULPH.
FACE, eruptions on face, comedones- ABROT, Eug, Jug-r, Nit-ac, SULPH.
FACE, eruptions on face, eczema – ANT-C, ARS, CROT-T, GRAPH, MEZ, VINC.
SKIN, eczema- AETH-M, ANAC, ANT-C, ARS, BERB, BOX, CALC, CANTH, CARB-AC, CIC, CLEM, CROT-T, GRAPH,HEP, KALI-AR, MANG-AC, MERC, MAG, OLND, PETR, PLB,PSOR, RHUS-T, SEP, SULPH-I, SULPH, VINC, VIOL- T.
SKIN, furuncle (boil)- ARN,BELL, BELL-P, CALC-PIC, PERR-I ,HEP, ICHTH, MED, MERC,PH- AC, PHYT, SIL,SULPH, TARENT-C
SKIN, RECURRENT TENDENCY- ARN, CALC, CALC-PIC, SULPH.
SKIN, leucoderma- ARS-S-F, Nat-m, Nit-ac, Sumb, zinc.
SKIN, pruritis (itching of skin) – AGAR, AMBR, ANAC, ANTIP, ARS, CARB-AC, CLEM, CROT-T, DOL, FAGO, GRAPH, HYDRC, LYC, MERC, MEZ, MORPH, PIX, RAD-BR, RHUS-T, RHUS-V, RUMX, SEP, SULPH, URT-U
SKIN, psoriasis – ARS, ARS-I, BORX, CARB-AC, CHRYSAR, GRAPH, KKALI-AR, KALI-BR, LYC, MANG-ACT, MERC, PETR, PHOS, SEP, SULPH, THYR.
SKIN, scabies (itch) – CROT-T, HEP, PSOR, SEP, SULPH.
SKIN, tinea favosa, favus – BROM, KALI-C, LYC, MEZ, SEP.
SKIN, tinea versicolor (chromophytosis) – CHRYSAR, NAT-AR, SEP.
SKIN, ulcers – ANAN, ANTHRACI, ARS, CALC, CALC-P, CALC-S, CALC-SIL, CAR-AC, CARB-AN, CARB-V, CLEM, ECHI, FL-AC, GAUL, GER, HEP, HYDR, KALI-BI, LACH, MERC, PHYT, SIL, SYPH.
SKIN, urticaria (hives, nettle rash) – ANT-C, APIS, ARS, ASTAC, BOMB-PR, BOV, CAMPH, CHOL, CIMIC, COP, DULC, FRAG, ICHTH, NAT-P, PULS, RHUS-T, SULPH, THIOS, URT-U.
SKIN, verruca (warts) – ANT-C, CALC, CAUST, DULC, FERRR-PIC, MAG-S, NAT-C, NIT-AC, SIL, THUJ.
CONCLUSION
Skin disorders are the outward reflection of the internal derangement of the body, therefore suppression of skin problems by means of topical solution or by other means isn’t the solution or not the right way to treat these problems. In homoeopathy, there are many repertories including clinical as well general, and these repertories contain an entire separate chapter of skin in which many rubrics of skin diseases and medicines related to its has been given. Rubrics of skin disorder can also be found under different chapters depending on the location or part is affected.
REFRENCES
- Khanna N. Dermatology and Sexually Transmitted Disease.1st ed. New delhi: Modern Publisher; 2002.
- Approach to skin lesions| Learn Pediatrics [internet]. 11march 2012. Available at:
https://learn.pediatrics.ubc.ca/body-systems/general-pediatrics/aproach-to-skin-lesions/
- Work related skin disease- OSHWIKI [internet]. 1june 2017. Available at:
https://oshwiki.eu/wiki/Work-related_skin_diseases
- Phatak S.R..A Concise Repertory of Homoeopathic Medicines. 4th ed. New Delhi: B. Jain Publishers (P) Ltd; 2009.
- Boericke W. New manual of Homoeopathic Materia Medica and repertory. 9th ed. New Delhi: B. Jain Publishers (P) Ltd; 2011.
ABOUT THE AUTHOR
Dr Yogyata Kashyap, MD Scholar, Dept. of Repertory,
Dr. M.P.K Homoeopathic Medical College, Homoeopathy University,
Jaipur.