Abstract
Hypertension remains one of the leading contributors to the global burden of disease. Blood pressure levels, which exhibit a normal distribution across the general population, are strongly associated with the risk of cardiovascular events, including stroke and coronary artery disease. The prevalence of hypertension rises significantly with advancing age. Effective blood pressure management plays a crucial role in reducing cardiovascular morbidity and mortality, lowering the incidence of acute coronary syndromes by 20–25%, stroke by 30–35%, and heart failure by nearly 50%. These statistics underscore the importance of early diagnosis, regular monitoring, and optimal therapeutic strategies in the prevention of hypertension-related complications.
Keywords: Essential hypertension, Secondary hypertension, systolic blood pressure, Diastolic blood pressure, Coronary artery disease, stroke.
Introduction
Definition
Blood pressure is defined as a lateral pressure exerted on the vessel wall by the flowing blood.
Hypertension is defined as a persistent elevation of arterial blood pressure, where systolic blood pressure (SBP) is ≥ 140 mm Hg and/or diastolic blood pressure (DBP) is ≥ 90 mm Hg, measured on at least two separate occasions under standardized conditions.
It can be classified as primary (essential) hypertension, where no specific cause is identifiable, or secondary hypertension, which results from an underlying, potentially reversible cause.
Primary (Essential )Hypertension
95% of hypertensive patients due to multiple genetic and environmental factors.
The onset between ages 25 and 50 years
uncommon before age 20 years.
Causes of Primary (Essential )Hypertension
- Overactivation of the sympathetic nervous and renin-angiotensin-aldosterone systems (RAAS)
- Blunting of the pressure-natriuresis relationship
- Variation in cardiovascular and renal development,
- Elevated intracellular sodium and calcium levels
Exacerbating Factors
- Obesity, sleep apnea, Increased salt intake, Excessive alcohol use, Cigarette smoking, Polycythemia, NSAID therapy ,Low potassium intake
Management For Primary (Essential )Hypertension
- Reduce weight
- Restrict salt intake
- Avoid use of alcohol & smoking
- Practice of Aerobic exercise
- Avoid unnecessary use of NSAID drugs
Secondary Hypertension
Caused by an underlying medical condition, such as kidney disease, hormonal disorders, or certain medications
Causes for secondary hypertension
- Alcohol, Obesity, Pregnancy
- Renal disease
- Parenchymal renal disease, particularly glomerulonephritis, Renal vascular disease, Polycystic kidney disease
- Endocrine disease
- Phaeochromocytoma, Cushing’s syndrome, Primary hyperaldosteronism (Conn syndrome),Hyperparathyroidism, Acromegaly, Primary hypothyroidism, Thyrotoxicosis, Liddle syndrome
- Drugs
- Coarctation of the aorta
Diagnosis of Hypertension
A single elevated blood pressure reading is not sufficient to establish the diagnosis of hypertension.
The 2017 guidelines from the American College of Cardiology and American Heart Association (ACC/AHA)
| Category | Systolic blood pressure (mmHg | Diastolic blood pressure (mmHg) |
| BLOOD PRESSURE
Optimal |
< 120 | <80 |
| Normal | < 130 | 85 |
| High normal | 130–139 | 85-89 |
| HYPERTENSION
Grade 1 (mild) |
140-159 | 90-99 |
| Grade 2 (moderate) | 160-179 | 100-109 |
| Grade 3(Severe) | ≥ 180 | >110 |
| ISOLATED SYSTOLIC HYPERTENSION
Grade 1 |
140-159 | <90 |
| Grade 2 | ≥ 160 | <90 |
Risk Factors For Hypertension
It is multifactorial, involving both genetic predispositions and environmental influences.
- Genetic Factors: Variations in genes such as the alpha-adducin gene increases renal tubular sodium reabsorption.
- Advancing Age: Rise progressively with age due to vascular remodelling and increased arterial stiffness.
- Environmental and Lifestyle Factors:
- High Dietary Sodium Intake: particularly in genetically predisposed individuals.
- Heavy Alcohol Consumption: (>30 mL of ethanol/day)
- Obesity: Central (abdominal) obesity is particularly associated with increased sympathetic activity, insulin resistance, and sodium retention.
- Physical Inactivity: Sedentary behaviour contributes to weight gain and endothelial dysfunction, promoting hypertension.
- Fetal Origins:
- Impaired Intrauterine Growth and Low Birth Weight: According to the Barker Hypothesis, suboptimal fetal nutrition and growth are linked to permanent changes in vascular structure and renal development, predisposing individuals to hypertension later in life.
Additionally, circadian patterns of blood pressure have critical prognostic implications:
- Normally, blood pressure declines during sleep — a phenomenon known as the “nocturnal dip”. The absence of this nocturnal dip (non-dipping pattern) is a powerful predictor of cardiovascular morbidity, particularly ischemic stroke and myocardial infarction.
- An exaggerated morning surge in blood pressure has been associated with an increased risk of cerebral haemorrhage and other adverse cardiovascular events.
|
How it mimics hypertension | Clues to differentiate |
| White coat hypertension | BP high only in clinical setting | Normal BP at home or ambulatory BP monitoring |
| Pheochromocytoma | Sudden high BP spikes, anxiety, sweating | Check plasma metanephrines |
| Cushing’s Syndrome | Persistent high BP, obesity, stretch marks | Test cortisol levels |
| Primary hyperaldosteronism | Hypertension + low potassium | Aldosterone/renin ratio test |
| Chronic kidney disease | High BP with abnormal kidney function | Elevated serum creatinine, abnormal urinalysis |
| Coarctation of aorta | High BP in arms, low in legs | Check BP difference in limbs, echocardiogram |
| Obstructive sleep apnea | Nocturnal hypertension, snoring, daytime sleepiness | Sleep study (polysomnography) |
| Medication-induced hypertension | Decongestants, steroids, NSAIDs, oral contraceptives | Careful drug history |
Clinical Findings
- SYMPTOMS
- Mild to moderate primary (essential) hypertension -asymptomatic, headache nonspecific.
- Hypertensive encephalopathy -headache, somnolence, and vomiting
- Focal neurologic deficits -cerebral infarction or hemorrhage. Subarachnoid hemorrhage – loss of consciousness and neck stiffness.
- LVH -angina and dyspnea.
- Aortic dissection or rupture – chest or abdominal pain.
- Cerebral involvement – thrombosis or hemorrhage
- SIGNS
- Osler sign—a palpable brachial or radial artery when the cuff is inflated above systolic pressure.
- copper or silver wire appearance in retinas
- A presystolic (S4 ) gallop due to decreased compliance of the LV
- Radial-femoral delay
- loss of peripheral pulses
- INVESTIGATIONS
| System | Test |
| Renal | Microscopic urinalysis, albumin excretion, serum BUN and/or creatinine |
| Endocrine | Serum sodium, potassium, calcium, ?TSH |
| Metabolic | Fasting blood glucose, total cholesterol, HDL and LDL
(often computed) cholesterol, triglycerides |
| Other | Hematocrit, electrocardiogram |
Abbreviations: BUN, blood urea nitrogen; HDL, high-density lipoprotein; LDL, low density lipoprotein; TSH, thyroid stimulating hormone.
- ECG AND CHEST RADIOGRAPHS
Electrocardiographic criteria are highly specific but not very sensitive for LVH
The “strain” pattern of ST–T wave changes is a sign of more advanced disease and is associated with a poor prognosis
- ECHOCARDIOGRAPHY
To evaluate clinical symptoms or signs of cardiac disease.
- DIAGNOSTIC STUDIES
24-hour urine free cortisol
urine or plasma metanephrines
plasma aldosterone and renin concentrations to screen for endocrine causes of hypertension.
Renal ultrasound will detect structural changes (such as polycystic kidneys, asymmetry, and hydronephrosis); increased echogenicity and reduced cortical volume are reliable indicators of advanced CKD.
Pathogenesis.
IN LARGER ARTERIES (>1mm in diameter)
The internal elastic lamina is thickened
Smooth muscle is hypertrophied
Fibrous tissue is deposited
The vessels dilate and become tortuous
Their walls become less compliant.
IN SMALLER ARTERIES ( (<1mm)
Hyaline arteriosclerosis occurs in the wall
The lumen narrows
Aneurysms may develop.
Widespread atheroma develops
Lead to coronary and cerebrovascular disease
If other risk factors are present. These structural changes in the vasculature often perpetuate and aggravate hypertension by increasing peripheral vascular resistance and reducing renal blood flow, thereby activating the renin–angiotensin–aldosterone axis.
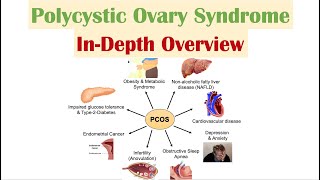
Complications of Hypertension
- Left ventricular failure in the absence of CAD
- Aortic aneurysm
- Peripheral artery disease
- Stroke.
- Retinal ischemia or infarction, (cotton wool’ exudates)
- Microaneurysms
- Hypertensive Kidney Disease
Management
- Non-drug therapy
- Correcting obesity, reducing alcohol intake, restricting salt intake, taking regular physical exercise, increasing consumption of fruit and vegetables , stopping smoking, Diet that is low in saturated fat
- Drug therapy
- Thiazides, ACE inhibitors, Angiotensin receptor blockers, Calcium channel antagonists, Beta-blockers, Combined β- and α-blockers, other vasodilators (Aspirin, Statins)
Homoeopathic Remedies For Hypertension
1.Crataegus Oxyacantha –Cardiac dropsy, incompetent valve, pulse rapid, irregular, angina pectoris.
- Natrum Muriaticum –palpitation, pulse full and slow, intermittent every third beats
- Aconitum Napellus –palpitation with anxiety, pulse fast, bounding, arterial tension, carditis
- Glonoinum –throbbing carotids, pulsation of the whole body to the fingertip, venous pulses.
- Baryta Carbonica –palpitation felt in head, aneurism, pulse slow, small, arteriosclerosis
- Iodum –heart feel squeezed, great weakness and faintness, palpitation <least exertion, pulsation in large arterial trunk
- Nux Vomica –palpitation on lying down, heart feels tired, angina pectoris
- 8. Lachesis – pulse weak, intermittent, slow ,irregular, carditis, restless, anxiety about heart
- Belladonna –throbbing in carotid and temporal arteries, pulse full hard, tense, violent palpitation
- Aurum Metallicum– sensation as if stopped beating of heart, oppression at heart, pulse rapid, feeble, irregular, venous congestion more to head and chest
Miasmatic Influences in Hypertension
- Psoric Miasm
- Characteristics: Functional disturbances without significant structural changes.
- Clinical Features: Labile blood pressure, stress-induced elevations, anxiety, and emotional hypersensitivity.
- Remedies: Aconitum napellus, Nux vomica, Ignatia amara.
- Sycotic Miasm
- Characteristics: Tendency towards overgrowth and accumulation.
- Clinical Features: Persistent hypertension, obesity, water retention, and metabolic syndrome.
- Remedies: Natrum sulphuricum, Thuja occidentalis, Lycopodium clavatum.
- Syphilitic Miasm
- Characteristics: Degenerative and destructive processes.
- Clinical Features: Malignant hypertension, end-organ damage, arteriosclerosis, and hemorrhagic tendencies.
- Remedies: Mercurius solubilis, Aurum metallicum, Plumbum metallicum.
4. Tubercular Miasm
- Characteristics: A combination of psoric and syphilitic traits, marked by rapid changes and susceptibility.
- Clinical Features: Fluctuating blood pressure, nervous excitability, and hemorrhagic episodes.
- Remedies: Phosphorus, Calcarea phosphorica, Tuberculinum.
Conclusion
Hypertension remains a significant global health concern; homoeopathy offers a complementary approach to managing this condition. By focusing on individualized treatment, addressing underlying causes, and promoting overall well-being, homoeopathy can serve as an adjunct to conventional methods. Though more research is needed to fully understand its efficacy, many individuals have found relief through holistic remedies. A balanced lifestyle, proper medical guidance, and personalized treatment plans remain essential for effectively controlling hypertension and enhancing long-term health.
References
- Barker DJP. Fetal Origins of Coronary Heart Disease. BMJ. 1995;311(6998):171–4.
- Jameson JL, Fauci AS, Kasper DL, Hauser SL, Loscalzo J, editors. Harrison’s Principles of Internal Medicine. 21st ed. New York: McGraw Hill; 2022.
- O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. Ambulatory Blood Pressure Monitoring in the 21st Century. J Clin Hypertens (Greenwich). 2018;20(7):1108–11.
- Papadakis MA, McPhee SJ, Rabow MW. CURRENT Medical Diagnosis & Treatment. 63rd ed. New York: McGraw Hill Inc; 2024.
- Phatak SR. Materia Medica of Homoeopathic Medicines. 2nd ed. New Delhi: B. Jain Publishers; 2007.
- Ralston SH, Penman ID, Strachan MWJ, Hobson RP, editors. Davidson’s Principles and Practice of Medicine. 24th ed. Edinburgh: Elsevier; 2022.
About the Author:
Dr. Priya James: MD Scholar Department of Practice of Medicine
Guide: Dr. G Rajachandra
MD ,Associate professor Department of Practice of Medicine
Father Muller Homoeopathic Medical College, Mangalore