Abstract: In the management of chyluria, most of the patients respond to dietary management, anti-filarial drugs and one or at the most two courses of sclerotherapy. Small number of patients who fail this treatment, chylo-lymphatic disconnection (open or laparoscopic) was a good surgical option with dependable long-term results. This case report supports the evidence that individualised homoeopathic medicine Thuja occidentalis may be useful in chyluria cases as it was used in the study done by CCRH (Central Council for Research in Homoeopathy) where Rhus toxicodendron, Apis mellifica, Sulphur and Thuja occidentalis were the most useful medicines and there is no need of surgical intervention like chylo-lymphatic disconnection. There is a better scope for the treatment of chyluria since the treatment is based on holistic and individualistic approach though it is grade C level IV evidence (level of evidence according to WHO) , this case report encourage to conduct further pilot study or RCT on chyluria.
Keywords: chyluria, individualised homoeopathic medicine, Thuja occidentalis.
Abbreviations: World Health Organization (WHO), Central Council of Research in Homoeopathy (CCRH), Wucheria bancrofti (W. bancrofti), randomized controlled trial (RCT) renal pelvic instillation of sclerosant (RPIS), ultrasonography (USG), kidney, ureter, bladder (KUB), high density lipoprotein (HDL), red blood cells (RBC), high power field (HPF).
Introduction:
Chyluria is endemic in South-east Asia, China, India, Japan, Taiwan and parts of Africa, Australia and South America. W. bancrofti infestation is responsible for >95% of parasitic chyluria in endemic regions [1], [2], [3], [4], [5], [6]. Although this disease is not life threatening, 5-10% of our patients have presented with considerable weight loss and weakness secondary to chronic chyluria. Chyluria is due to the passage of chyle into the urine giving it a typical milky appearance. Filariasis is the commonest cause, which is endemic problem in various Indian states. On chyluria, a study was done by A. Suri and A. Kumar at Department of Urology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India[7]. Over the 18 years, they have managed about 600 cases of chyluria. The patients presented with various complaints like passage of white colour urine, haematuria (haematochyluria), passage of chylous clots in urine and dysuria. Treatment was customised by them according to severity of chyluria. In patients presenting with occasional history of chyluria, they prescribed dietary modifications like high protein low fat diet, promoting medium chain triglyceride intake along with diethylcarbamazine for 3 weeks. Those not responding to the treatment were subjected to renal pelvic instillation of sclerosant (RPIS). In the management of chyluria they said that most of the patients respond to dietary management, antifilarial drugs and one or at the most two courses of sclerotherapy. Small number of patients who fail this treatment, chylolymphatic disconnection (open or laparoscopic) was a good surgical option with dependable long-term results.
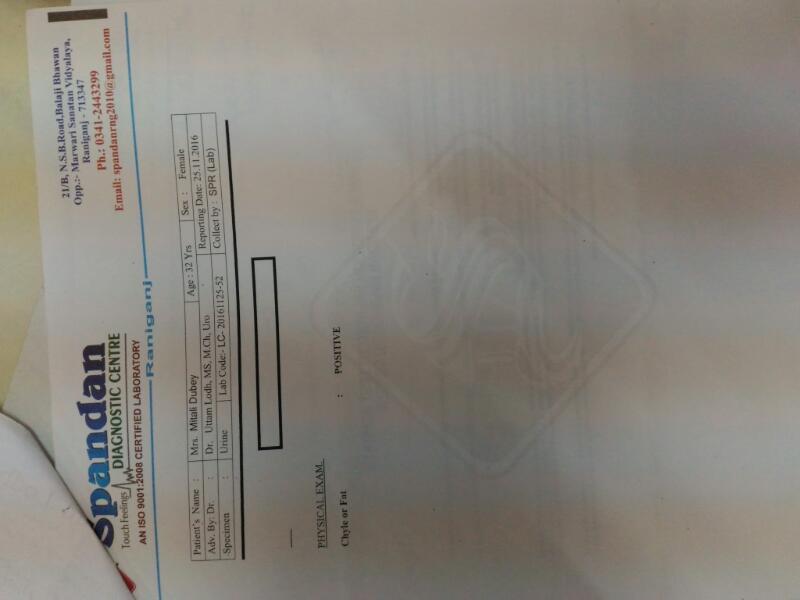
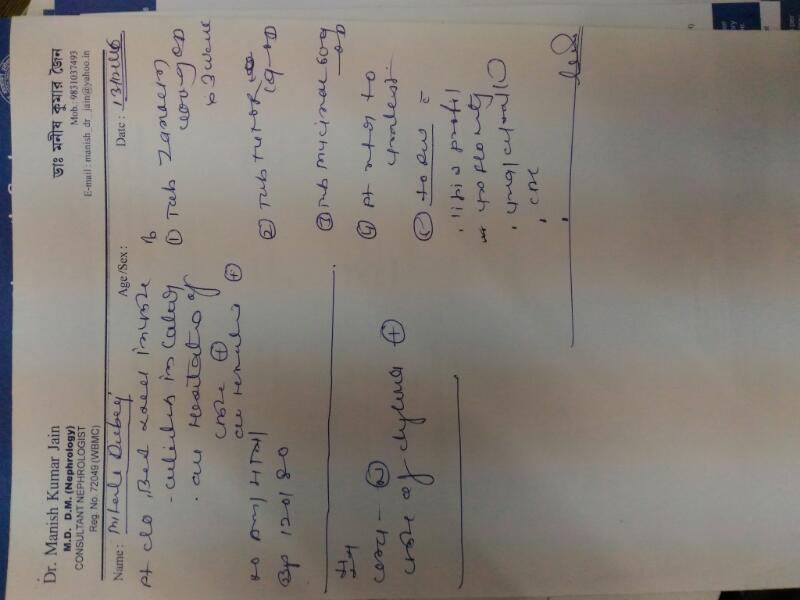
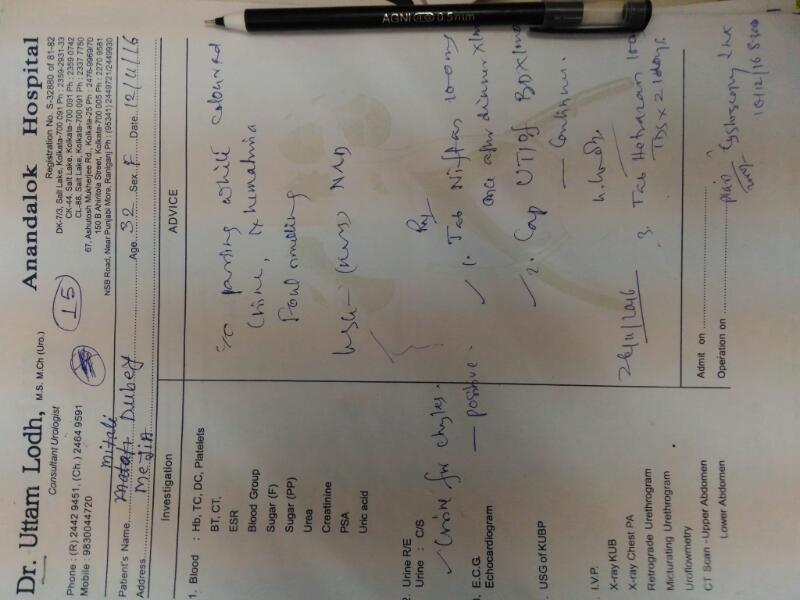
Here is a case of 32 years lady who came with complaint of milky urine. USG of KUB and lower abdomen done on 09.11.2016 was within normal limit. On 14.12.2016, biochemical report of blood plasma revealed normal serum urea, creatinine, cholesterol, triglyceride levels. Serum sodium level was normal though serum potassium level slightly increased 6 mmol/L (normal range-3.5-5.2 mmol/L) and ratio of total cholesterol and HDL level slightly increased 4.67 (normal up to 4.5). Report on haematology shows within normal limits except haemoglobin which was 11.9 gm/dl. These haematology and biochemical report of blood plasma on 14.12.2016 excluded the renal pathology if any. Urine culture and sensitivity isolated bacteria escherichia coli colony count 70,000/r, and by urine routine microscopy, it was revealed that specific gravity was 1.025; pale coloured urine and hazy on physical examination; chemically urine was acidic with reaction; albumin present; blood positive; RBC plenty/HPF which indicates grade III chyluria, i.e. haematochyluria but ruled out other causes of milky white urine like phosphaturia (clears on adding 10% acetic acid), amorphous urates, severe pyuria, lipiduria secondary to fat embolism, and pseudochylous urine. On the basis of homoeopathic principles of prescribing, the case was prescribed on 17.12.2016 with Thuja occidentalis 30/ one dose with Thuja occidentalis 200/ one dose on subsequent next day with placebo for 15 days.
| Case taking | |
| Present complaint | Hot, burning urine with cloudy milky offensive. On enquiry, it was revealed that splitting of stream also present. The complaint was since 6 months. |
| Mental general | Mistakes in writing |
| Physical general | Desire – cold food |
| Aversion – potato | |
| Thirsty | |
| Constipation | |
| Perspiration all over body except scalp | |
| Particular symptom | Urine – hot, burning |
| Urine – cloudy | |
| Urine – strong odour | |
| Urination – frequent | |
| Forked stream | |
| Objective symptom | Wart on face |
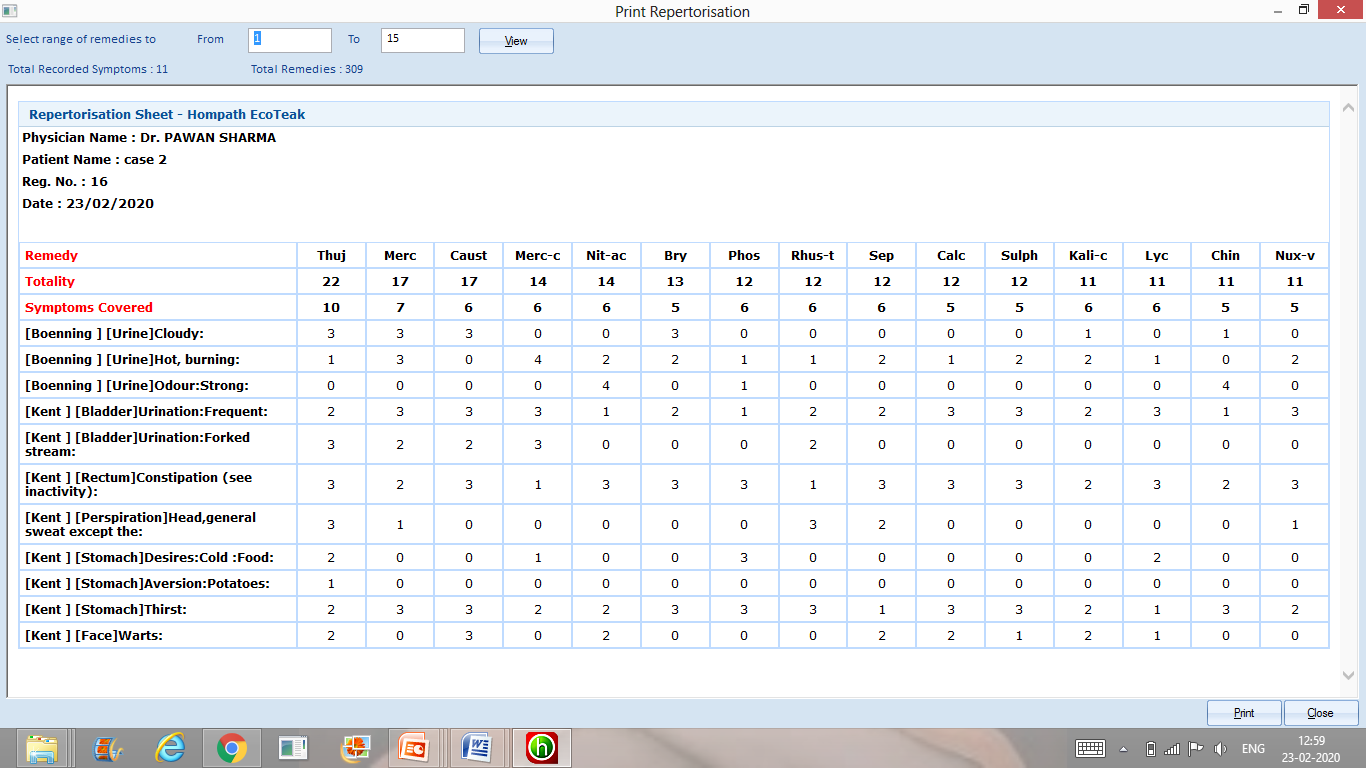
After repertorisation, Thuja occidentalis, Merc sol., Causticum came out to be the best indicated drugs for prescription Kent’s Repertory with help of Hompath Eco-tek. After considering the predominant miasm, the best remedy ruled out was Thuja occidentalis whichcovered 10 symptoms among 11 symptoms with highest mark 22.
| Urine R/E | Follow up | |
| 29.12 2016 | Urine-blood positive RBC 2-4/ HPF Specific gravity 1.015 Physical examination- straw colour | 31.12.2016- On the basis of current totality again Thuja Occidentalis 0/7 14 doses was prescribed at every alternative day along with placebo. |
| 27.01.2017 | Blood – nil RBC – nil Specific gravity – 1.020 Physical examination- pale yellow colour | 28.01.17- On the basis of current totality again Thuja Occidentalis 0/9 14 doses was prescribed at every alternative day along with placebo. |
| 25.02.2017 | Blood – nil RBC – nil Specific gravity – 1.015 Physical examination- straw colour | 25.02.17- On the basis of current totality, again Thuja occidentalis 0/7 – 14 doses was prescribed at every alternative day along with placebo. |
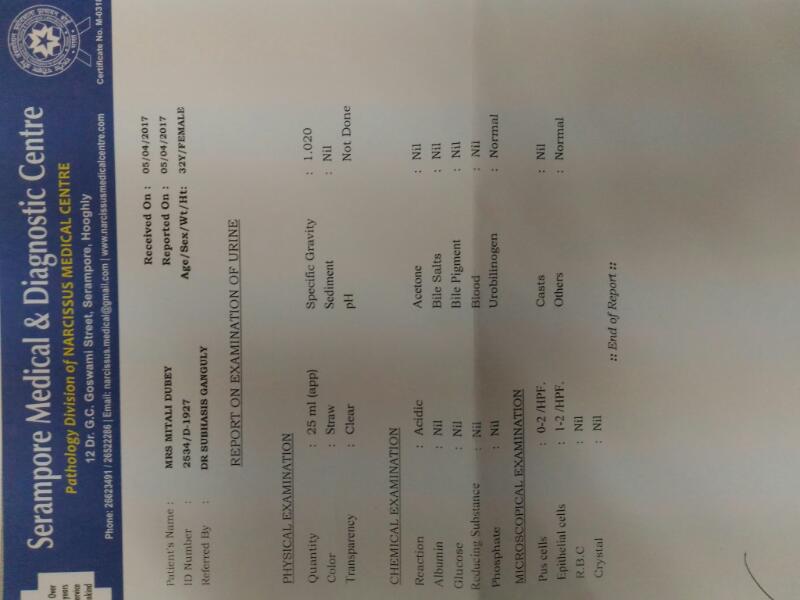
| 05.04.2017 | All within normal limits | 10.04.2017- placebo given for 1 month |
On further reporting of patient on 31.12.2016, she was better with her urinary complaints and the reports of urine examination done on 29.12.2016 was chemical examination of urine -blood positive and RBC 2-4/ HPF along with specific gravity 1.015 with straw coloured urine on physical examination.
On the basis of current totality again Thuja occidentalis 0/7-14 doses was prescribed at every alternative day along with placebo. This time fifty millesemal potency was prescribed according to rules of homoeopathic posology and repetition. After one month, the reports of urine examination done on 27.01.2017 reported that blood nil in chemical examination; RBC nil on chemical examination and specific gravity 1.020 with pale yellow colour urine on physical examination. In clinical correlation, patient was also better than before but after one month further reports of urine examination done on 25.02.2017 was blood nil in chemical examination; RBC nil on chemical examination and specific gravity 1.015 with straw coloured urine on physical examination.
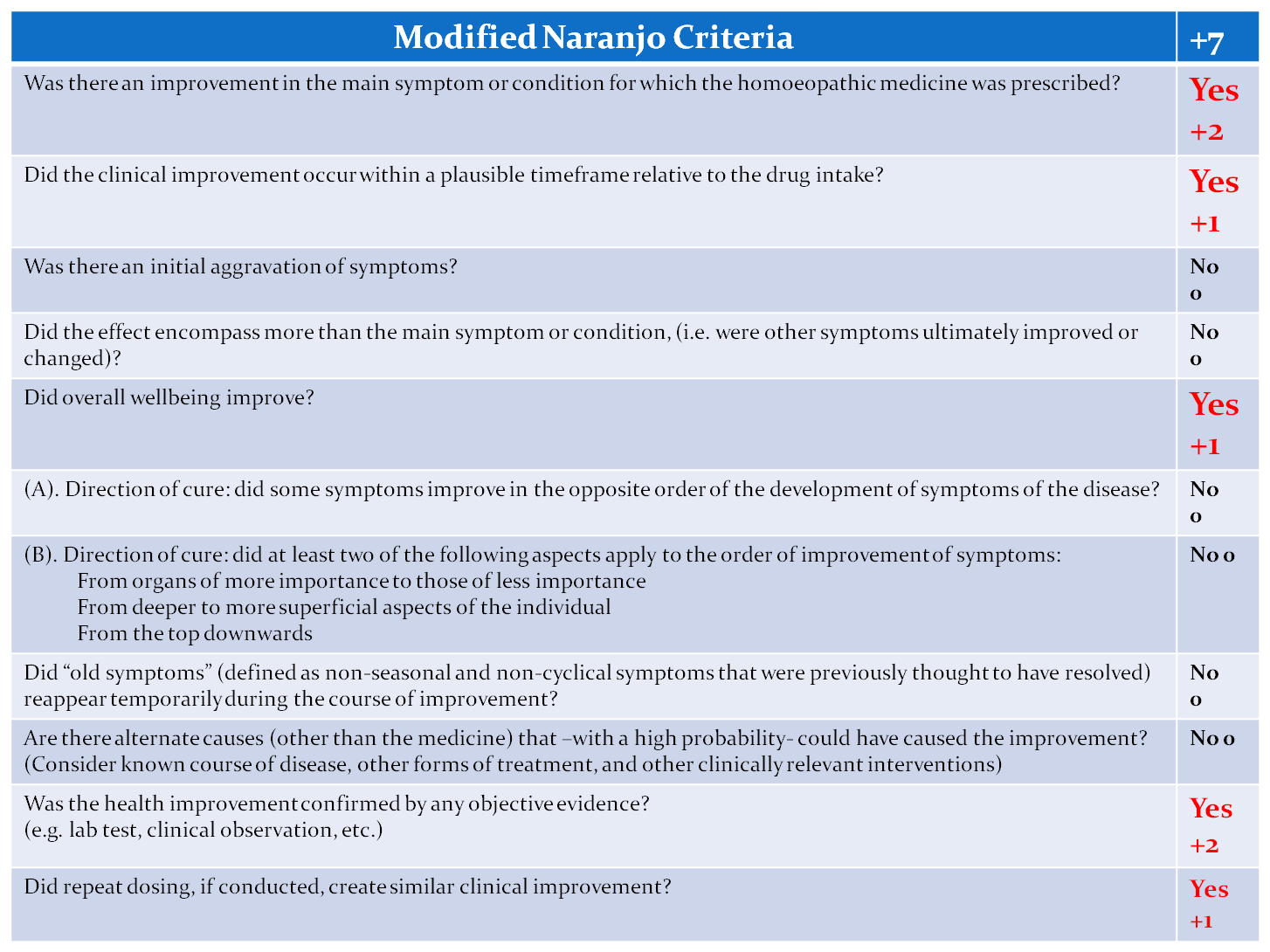
Modified naranjo criteria as proposed by the United States Homoeopathic Pharmacopoeia clinical data working group: these adapted algorithm enables us to increase certainty that the medicine cause improvement of the patient for establishing a causal relationship between cure and homoeopathic medicine, we have used this algorithm. In the above modified naranjo criteria, the total score is +7, which indicates that there is definitive causal attribution between patient and homoeopathic treatment[8].
Discussion: This case report supports the evidence that Thuja occidentalis may be useful in chyluria cases as it was used in above mentioned study done by CCRH[9],[10], where Rhus toxicodendron, Apis mellifica, Sulphur and Thuja occidentalis were the most useful medicines[11].
Again there is no need of surgical intervention, chylo-lymphatic disconnection as done in some of patients who fail this medicine treatment at SGPGI study by A Suri et al.
Conclusion: In this case report, it can be concluded that homoeopathic medicines are of importance in managing chyluria and can help the patient to take a new lease on life. There is a better scope for the treatment of chyluria since the treatment is based on holistic and individualistic approach but to establish their proper effects a long-term trials are required on large sample size in future. Though it is grade C level IV evidence, this case report encourage to conduct further pilot study or RCT on chyluria.
References:
[1] Dalela D, Kumar A, Ahlawat R, Goel TC, Mishra VK, Chandra H. Routine radio-imaging in filarial chyluria-is it necessary in developing countries? Br J Urol 1992;69:291-3. [2]Goel S, Mandhani A, Kumar A, Srivastava A, Kapoor R, Gogoi S, Bhandari M. et al. Is povidone iodine an alternative to silver nitrate for renal pelvic instillation sclerotherapy in chyluria? 2004 BJU Intenational [3] Dash SC, Bhargav Y, Saxena S, Agarwal SK, Tiwari SC, Dinda A. Acute renalfailure and renal papillary necrosisfollowing instillation of silver nitrate fortreatment of chyluria.Nephrol DialTransplant1996;11:1841-2 [4] Srivastava DN, Yadav S, Hemal AK, Berry M . Arterial haemorrhage followinginstillation of silver nitrate in chyluria:treatment by coil embolization.AustralasRadiol1998;42:234-5 [5] Gulati MS, Sharma R, Kapoor A, Berry M . Pelvi-calyceal cast formation following silver nitrate treatment for chyluria. Australas Radiol 1999;43:102-3 [6] Mandhani A, Kapoor R, Gupta RK, Rao HS . Can silver nitrate instillation for the treatment of chyluria be fatal? Br J Urol 1998;82:926-7. [7] Suri A, Kumar A. Chyluria – SGPGI experience. Indian J Urol 2005;21:59-62. [8] Rutten L. Prognostic factor research in Homoeopathy. Indian J Res Homoeopathy 2016;10:59-65 [9] Subramanyam VR, Mishra N, Rai Y, Rakshit G, and Pattnaik NM. Homoeopathic treatment of filariasis: Experience in an Indian rural setting. British Homoeopathic Journal 1990; 79(3):157-160. [10] Mishra N, Murthy GSN, Bhanumurthy K, Mai PC, Ramesh D, Ghosh SK et al. Filariasis. Clinical Research Studies -Series 1. New Delhi: CCRH; 2008:53-66. [11] Kumar A and Mishra N. Effect of homoeopathic treatment on filariasis: A single blind 69-month follow up study in an endemic village in Orissa. British Homoeopathic Journal 1994; 83(4): 216-9
About Author:
[1] Prof. (Dr) Subhasish Ganguly– HOD (UG & PG), Department Of Organon Of Medicine, D. N. De Homoeopathic Medical College & Hospital
[2] Dr Pawan Sharma- Research Officer (H)/ Scientist-1; Regional Research Institute for Homoeopathy, Guwhati under CCRH, Ministry of AYUSH, Govt. of India.
[3] Dr Tanya Aggarwal –Corresponding author; Asst. Secretary (Tech), Central Council of Homoeopathy; formerly Senior Research Fellow, CCRH headquarters, New Delhi, Ministry of AYUSH, Govt. of India. Formerly PGT, Deptt of Practice of Medicine, Nehru Homoeopathic Medical College & Hospital.