ABSTRACT
Background:
Impetigo is one of the most common superficial bacterial skin infections affecting children
worldwide. Both Impetigo contagiosa (non-bullous) and Bullous impetigo present with high
infectivity, discomfort, and cosmetic concerns. Conventional therapy primarily relies on
topical and systemic antibiotics. However, rising antimicrobial resistance has increased
interest in complementary approaches, including Homoeopathy.
Aim:
To review the clinical presentation, pathophysiology, and evidence-based homoeopathic
management of impetigo contagiosa and bullous impetigo.
Methods:
A narrative review of published dermatological, microbiological, and homoeopathic
literature, including classical homoeopathic texts, repertories, and recent clinical
observations.
Results:
Homoeopathic medicines—selected based on totality of symptoms, constitution, and
miasmatic background—demonstrate supportive benefit in reducing suppuration, crusting,
recurrence, and healing time. Commonly indicated remedies include Antimonium crudum,
Graphites, Hepar sulphuris, Mercurius solubilis, Rhus toxicodendron, and Sulphur. Evidence
is limited but promising.
Conclusion:
Homoeopathy offers a safe, individualized therapeutic option in impetigo, particularly in
recurrent, mild-to-moderate, and antibiotic-resistant cases. Larger controlled studies are
recommended.
INTRODUCTION
Impetigo is a highly contagious superficial infection of the epidermis, predominantly
affecting children aged 2–10 years. The condition is caused by Staphylococcus aureus,
Streptococcus pyogenes, or both. Overcrowding, poor hygiene, insect bites, pre-existing
dermatoses, and warm–humid climates contribute to its spread.
Two major clinical forms are recognized:
1. Impetigo contagiosa (Non-bullous impetigo) – accounting for 70% of cases.
2. Bullous impetigo – caused exclusively by S. aureus producing exfoliative toxins.
Homoeopathy has historically managed infectious skin conditions based on symptom
similarity, host susceptibility, and miasmatic background. This article reviews each form of
impetigo and summarizes homoeopathic perspectives and therapeutics.
EPIDEMIOLOGY [1]
• Impetigo accounts for over 100 million cases globally per year.
• Peak incidence: 2–5 years of age.
• More common in tropical and low socioeconomic settings.
• Bullous impetigo is less common but presents more acutely in infants.
ETIOLOGY & PATHOGENESIS [2]1. Causative organisms:- Staphylococcus aureus – primary organism, especially for bullous
type, Streptococcus pyogenes – common in non-bullous impetigo.
2. Mechanism
Bacteria invade superficial epidermis through:- [2] Minor trauma, Insect bites, Eczema,
Scabies, Allergic rashes
Bullous impetigo:- Caused by S. aureus exfoliative toxins A and B → intraepidermal
cleavage → flaccid bullae.
3. Factors favouring infection- Warm & humid weather, Poor hygiene, Crowding,
malnutrition, Immune suppression
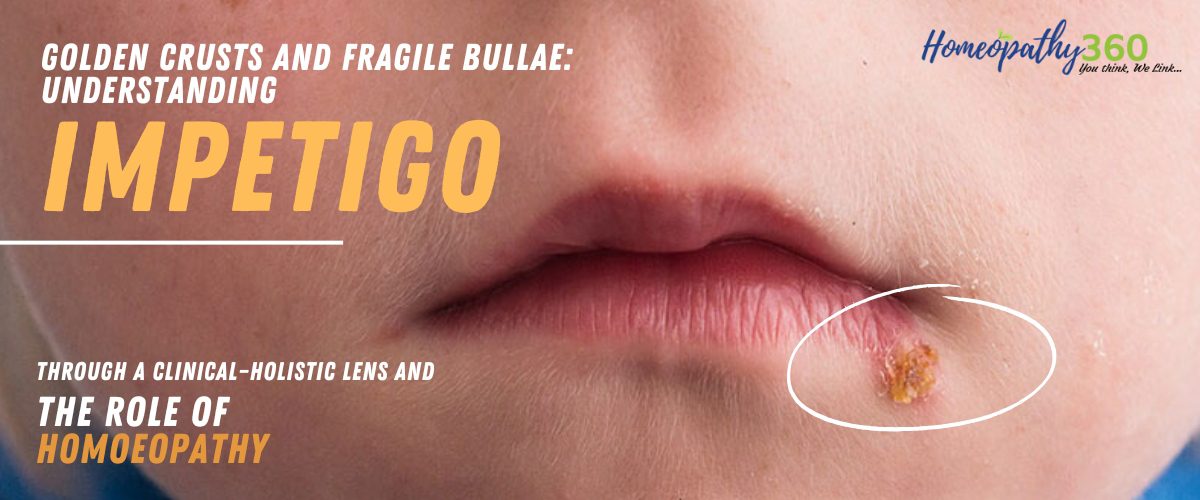
CLINICAL FEATURES [3]A. Impetigo Contagiosa (Non-bullous impetigo)
• Begins as small vesicles → rupture → form golden-yellow honey-coloured crusts
• Common on face, nose, mouth, extremities
• Lesions may be itchy and mildly painful
• Regional lymphadenopathy may occur
B. Bullous Impetigo
• Larger flaccid, thin-walled bullae
• Typically on trunk, buttocks, diaper area
• Filled with clear → turbid fluid
• After rupture → thin brown crust
• Systemic symptoms: fever, irritability (common in infants)
DIFFERENTIAL DIAGNOSIS [3]Condition Key Features Condition
Herpes simplex grouped vesicles, burning,
recurrence
Herpes simplex
Varicella successive crops of papules &
vesicles
Varicella
Eczema herpeticum painful monomorphic vesicles Eczema herpeticum
Contact dermatitis eczematous plaques, allergen
exposure
Contact dermatitis
Scabies with burrows, severe itching Scabies with secondary
secondary infection infection
INVESTIGATIONS [3]
Usually a clinical diagnosis.
Investigations may include:
i. Bacterial culture & sensitivity (recurrent/severe cases)
ii. CBC in extensive lesions
iii. Glucose levels in diabetics
iv. Patch testing for chronic or recurrent case
CONVENTIONAL MANAGEMENT [2] (Brief)
i. Topical antibiotics: Mupirocin, Fusidic acid
ii. Oral antibiotics: Cloxacillin, Amoxicillin-clavulanate, Cefalexin
iii. Antiseptic washes: chlorhexidine
iv. Addressing hygiene and environmental factors
HOMOEOPATHIC MANAGEMENT [4,5,6,7,8]Homoeopathy focuses on:
1. Symptom similarity (similimum)
2. Collective totality of physical + mental symptoms
3. Constitutional and miasmatic background
4. Chronic tendency to skin infections
Below is a detailed review of commonly effective remedies.
1. Antimonium Crudum
• Pustular eruptions with thick honey-colored crusts
• Irritability, aversion to touch
• Worse: heat, bathing
• Tongue: thick white coating
• Indicated in: non-bullous impetigo with crusting and excoriation.
2. Graphites
• Thick, sticky, honey-like discharge
• Cracks behind ears, at mouth corners
• Eruptions ooze a viscid, glutinous exudate
• Suited to obese, chilly, constipated patients
3. Hepar Sulphuris
• Painful pustules → exquisite sensitivity
• Early suppuration tendency
• Child irritable, over-sensitive
• Cold aggravation
• Indicated in: rapidly spreading impetigo or indurated pustules.
4. Mercurius Solubilis
• Profuse purulent discharge
• Offensive odor from lesions
• Increased salivation, perspiration
• Worse at night
• Useful in: spreading lesions with offensive exudation.
5. Rhus Toxicodendron
• Vesicles with thick serous discharge
• Red, itchy, burning lesions
• Worse cold & wet weather
• Useful when impetigo is secondary to eczema or insect bites
6. Sulphur
• Recurrent infections
• Itching, scratching → burning
• Unhealthy skin, slow healing
• Child dirty-looking, dislikes bathing
• A major constitutional anti-psoric remedy.
ADJUNCTIVE HOMOEOPATHIC CARE
• Calendula Q (topical): promotes granulation, prevents superinfection
• Hygiene measures:
• Clean with normal saline
• Keep nails short
• Avoid sharing towels
EVIDENCE & CLINICAL OBSERVATIONS [8]Although large randomized trials are limited, multiple smaller clinical observations and case
series suggest: Faster drying of lesions, Reduced crust formation, Shorter healing time,
Reduction in recurrence, Avoiding unnecessary antibiotic use.
Classical homoeopathic literature strongly supports individualized treatment for pustular and
contagious skin diseases.
DISCUSSION
Impetigo remains a common pediatric infection with high transmissibility. The emergence of
antimicrobial-resistant S. aureus (MRSA) highlights the need for safe adjunctive or
alternative treatments. Homoeopathy offers individualized care addressing not only the lesion
but the patient’s constitution, susceptibility, and recurrent tendency. [2]
Many remedies—especially Graphites, Hepar sulphuris, Mercurius, and Rhus
tox—correspond closely to the characteristic appearance of impetigo. Constitutional remedies
such as Sulphur may prevent recurrence. However, homoeopathy should be integrated with
proper hygiene, nutrition, and (when required) antibiotics in severe cases. [6,7]CONCLUSION
Impetigo contagiosa and bullous impetigo are common yet highly manageable skin
infections. Homoeopathy provides a safe, individualized therapeutic approach that can reduce
symptom severity, recurrence, and dependence on antibiotics. More high-quality clinical
trials are needed to validate efficacy. Combined with hygienic measures, homoeopathy can be
an effective complementary therapy in both children and adults.
REFERENCES
1. Bowen AC, et al. The global epidemiology of impetigo. Clin Microbiol Rev. 2015.
2. Koning S, et al. Interventions for impetigo. Cochrane Database Syst Rev. 2012.
3. World Health Organization. Bacterial skin infections in children. WHO Report.
4. Boericke. W, Boericke’s New Manual of Homoeopathic Materia Medica with
repertory, New Delhi: B. Jain Publishers; 2015. ISBN: 978-81-319-0184-7
5. Kent JT. Kent's repertory of the Homoeopathic Materia Medica. Reprint edition. New
Delhi: B. Jain Publishers (P) Ltd; 2017
6. Roberts H. A. The Principal and art of cure by homoeopathy. New Delhi: В. Jain
publishers; Reprint Edition 2008, 2009
7. Hahnemann S. Organon of medicine art, 5 th edition. New Delhi, B Jain, Publishers;
2010
8. Allen HC. Keynotes and characteristics with comparisons of Materia Medica. 10 th ed.
New Delhi: B Jain Publishers; 1993
9. Stevenson G. Homoeopathy in infectious skin disorders. J Dermatol Homeopath.
10. Kumar P. Impetigo in children: clinical overview. Indian J Dermatol.
About Authors-
Dr. Ashok Yadav, Professor, Department of Practice of Medicine, Dr. M.P.K. Homoeopathic
Medical College, Hospital & Research Centre, Homoeopathy University, Jaipur, Rajasthan,
India
Dr. Virendra Chauhan, Associate Professor, Department of Practice of Medicine, Dr. M.P.K.
Homoeopathic Medical College, Hospital & Research Centre, Homoeopathy University,
Jaipur, Rajasthan, India
Dr. Mansi Saini, MD scholar, Department of Practice of Medicine, Dr. M.P.K. Homoeopathic
Medical College, Hospital & Research Centre, Homoeopathy University, Jaipur, Rajasthan,
India
Dr. Yashaswi Choudhary, MD scholar, Department of Practice of Medicine, Dr. M.P.K.
Homoeopathic Medical College, Hospital & Research Centre, Homoeopathy University,
Jaipur, Rajasthan, India