Introduction
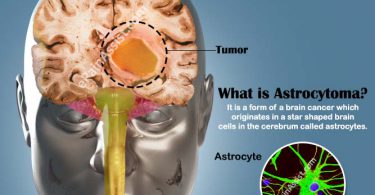
The term “psychosomatic” originates from the Greek words “psyche” (mind) and “soma” (body), indicating a condition that involves both mental and physical aspects. These disorders result from an intricate interplay between psychological stress or trauma and physical symptoms, often exacerbating existing medical conditions.
Common psychosomatic disorders encompass conditions such as Irritable Bowel Syndrome (IBS), Fibromyalgia, Psychogenic Non-Epileptic Seizures (PNES), Somatization Disorder, Conversion Disorder, and Tension Headaches and Migraines.
In this case study we will be dealing with tension headaches. Understanding tension headaches is essential for effective treatment, as their etiology remains incompletely understood. The initial attribution of tension headaches solely to muscle tension has been debunked. Anxiety surrounding the headache itself can perpetuate symptoms, instilling fear of underlying serious conditions in patients.
Recent studies have scrutinized the role of personality traits in such cases, highlighting heightened stress susceptibility in patients, particularly women, often coupled with neuroticism traits. Therefore, evaluations of migraine sufferers should encompass stress susceptibility, life events, and associated psychosomatic ailments.
Conventional treatments like painkillers frequently yield inadequate results and pose risks of long-term side effects, underscoring the need for alternative acute and preventive therapies. Here comes the role of Homeopathy, as it presents a promising avenue for enhancing the psychotherapeutic process, offering safe, gentle, non-toxic remedies grounded in holistic principles, as delineated in the aphorism 225 of the 6th edition of the Organon of Medicine.
Here, we present a case of psychosomatic headache with the homoeopathic constitutional medicine, which was selected on the basis of the totality of symptoms.
CASE REPORT
A tall, lean and thin 42 years old housewife, residing in Munirka, Delhi, presented with the following complaints on 22nd November, 2022 :-
PRESENTING COMPLAINTS:
PAIN IN HEAD – SINCE 7-8 MONTHS
FLATULENCE – SINCE 6-7 MONTHS
DIFFICULTY IN SLEEPING – SINCE 2 WEEKS
HISTORY OF PRESENT COMPLAINTS:
PAIN IN HEAD – SINCE 7-8
MONTHSFLATULENCE – SINCE 6-7
MONTHS DIFFICULTY IN SLEEPING – SINCE 2 WEEKS
HISTORY OF PRESENT COMPLAINTS:
PAIN IN HEAD
ONSET: Gradual
LOCATION: – Above left eye, alternating sides
EXTENSION: not specific
AURA: absent
CHARACTER OF PAIN: – Bursting, numb feeling
FREQUENCY: Thrice a week
INTENSITY: INTENSE
TRIGERING FACTOR: thinking too much about everything
INTENSITY: INTENSE
TRIGERING FACTOR: thinking too much about everything
MODALITY:
| Type of Modality | Aggravation | Amelioration |
| Time | Evening | – |
| Weather change | – | Open air |
| Positional change | Lying on left side | – |
| External stimuli | – | Dark room |
| Any other | Eating, unsatisfactory stools | Tight bandage |
CONCOMITANTS: Flatulence
PAST HISTORY: –
| Patient only took allopathic painkillers for her headache PERSONAL & SOCIAL HISTORY: -DEVELOPMENTAL LANDMARKS: On time ADDICTIONS: – Nothing specific DIET: Vegetarian MARITAL STATUS: Married HABBIT:- None as such EXERCISE: Frequently OCCUPATION: Housewife ENVIRONMENT AT HOME: Stressful due to death of father in-law and brother in-law FAMILY HISTORY: Father: Died due to asthmatic attack Mother: Alive and have hypertension Siblings: 1 Elder brother- asthmatic GYANECOLOGICAL HISTORY: – LAST MENSTRUAL PERIOD (LMP) – 14/02/2023 MENARCHE – Delayed, 16 years (took allopathic medicine for menarche) CYCLE – Early, 25 days DURATION -3-4 days CHARACTER OF FLOW – Dark and clotted, uneven, sometimes heavy PAIN – Present, unbearable in abdomen and back INTERMENSTRUAL BLEEDING – Absent LEUCORRHOEA – Present, stains linen white, without any odour and itching ANY OTHER ASSOCIATED COMPLAINT- N.S OBSTETRICAL HISTORY: – G – P – 1 L – 1 A – 1(spontaneous abortion at 2-3rd week) GENERALITIESPHYSICAL GENERALS: -THERMAL REACTION – Season: Likes winter. – Clothing: 2 Layers – Food & drinks: At normal temperature – Bathing: According to the weather – Fanning: from distance APPETITE – Decreased since 4 months (1chapati/meal) THIRST – Decreased since 4 months (1-2 glass/day) DESIRES – Spicy (2+), Salty (1+), Rice AVERSION – N.S URINE – D (4-5) N (0-1). No excessive odour and itching STOOL – D (1-2) N (0), Unsatisfactory stools Flatulence, belching with sour eructation SLEEP – Disturbed due to overthinking DREAMS – N.S PERSPIRATION – on calves, non-staining, non-offensive MENTAL GENERALS: – • The patient, a native of Delhi, completed her education and was employed as a teacher in a school. Approximately 1-2 years ago, she had to resign from her position due to her son’s exams, and now she desires to return to work. However, recent family bereavements have caused her significant stress, hindering her ability to resume her employment. • Over the past 1-2 months, the patient has noticed she has difficulty in remembering things. • She has experienced sorrow following the deaths of her father in 2009 and her cousin sister in 2016. • The patient is sociable and adept at forming friendships. • Her demeanor is characterized by politeness and empathy, often getting emotional and shedding tears upon hearing others’ troubles. • In moments of anger, she struggles to express herself verbally and used to resort to self-inflicted harm, though she has since learned to manage her anger and refrain from self-injury. • She becomes upset when witnessing her in-laws consume alcohol and engage in altercations. • Tears come easily to the patient, and she finds solace in receiving comfort from others. FINAL DIAGNOSIS: TENSION TYPE HEADACHE TOTALITY OF SYMPTOMS: Pain in head- above left eye, left temple. Sensation- bursting/ numb feeling.>tight bandage, dark room.<unsatisfactory stools, eating. Flatulence, no relief from belching. Sour eructation. Feels heavy in the abdomen. Talkative. Sympathetic. Desire to harm/ to be violent to herself. Feels better after consolation. REPERTORIAL TOTALITY: Mind – consolation ameliorates Mind – self destructive Mind – loquacity Mind – sympathetic Head – pain- temples – left – bursting pain Head – pain- darkness- amelioration Head – pain – temples – eating – aggravation Head – pain – temples – pressure – amelioration Head – pain – temples – stools – difficult – during Stomach – eructation – relief ; without Abdomen – flatulence Sleep – disturbed – thoughts; by Generals – food & drinks – rice – desires Generals – food & drinks – spices – desires REPERTORIAL ANALYSIS: Phos. – 15/7 Chin. – 14/7 Staph. – 8/7 Vanil. – 8/8 Lyc. – 10/7 Ruta – 7/7 Puls. – 12/6 PRESCRIPTION Puls 200/ 2 doses SL 30/ TDS/ 10 days | ||
Other than the medicines prescribed above general management including auxiliary measures were also advised.
Advice:
Healthy and balanced diet.
Sound sleep of 8 hours.
Yoga and Meditation of 30 minutes daily.
+4 Cured /Back to normal
+3 Major Improvement
+2 Moderate improvement, affecting daily living
+1 Slight improvement, no effect on daily living
0 No change/Unsure
-1 Slight deterioration, no effect on daily living
-2 Moderate deterioration, affecting daily living
-3 Major deterioration
-4 Disastrous deterioration Patient was asked to fill the ORDIL Form
Please complete the 3 boxes using the scale shown above:
The main complaint for which you came for treatment ……………. +3
Your overall coping with the problem …………… +3
Your overall well-being ——— +4
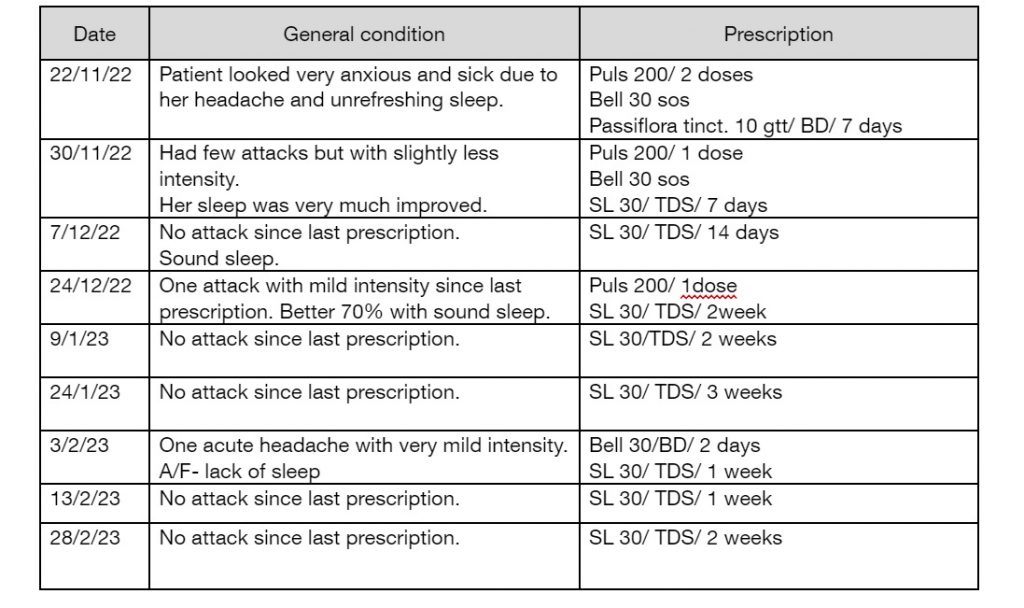
Therefore, based on the totality of the symptoms presented, PULSATILLA 200 was recommended. The patient exhibited a favorable response and showed gradual improvement thereafter.
CONCLUSION:
The situation was examined, revealing that the patient’s constant headaches and sleep disturbances stemmed from emotional stress within the household, compounded by the loss of family members and the inability to return to work. This scenario aligns with the classic definition of a psychosomatic disorder, as outlined in §225 of the 6th edition of the Organon of Medicine. “There are, however, as has just been stated, certainly a few emotional diseases which have not merely been developed INTO that form out of corporeal diseases, but which, in an inverse manner, the body being but slightly indisposed, originate and are kept up by emotional causes, such as continued anxiety, worry, vexation, wrongs and the frequent occurrence of great fear and fright. This kind of emotional disease in time destroys the corporeal health, often to a great degree.”
Therefore, based on the totality of the symptoms presented, PULSATILLA 200 was recommended. The patient exhibited a favourable response and showed gradual improvement thereafter.
REFERENCES:
Migraine Headache – Marco A. Pescador Ruschel; Orlando De Jesus
Medicine 24th edition – Davidson
Harrison’s principles of internal medicine- edition 21st
Organon of medicine by Dr S. Hahneman 6th edition (translated by Dr William Boericke)
Kent’s Repertory
Lectures on Homoeopathic Materia Medica – J.T. Kent
Pearce J. Migraine: A psychosomatic disorder. Headache.
Synthesis e-repertory