Complete Resolution of Dystonia with Individualized Homoeopathic Treatment : A Case Report
Abstract:
Introduction: Dystonia is a neurological disorder classified as a hyperkinetic movement disorder, characterized by sustained or intermittent muscle contractions leading to involuntary, repetitive movements, abnormal postures, or both in the affected body regions. Effective management of dystonia requires accurate diagnosis followed by appropriate treatment. Conventional approaches, including oral medications, intramuscular botulinum toxin injections, and deep brain stimulation, provide symptomatic relief but often necessitate repeated administration with increasing dosages, posing significant emotional and financial burdens on patients. In contrast, a holistic treatment approach integrating individualized homoeopathic medicine, personalized movement and breathing exercises, music therapy, and meditation may facilitate comprehensive recovery, promoting overall well-being and long-term improvement.
Case summary: In this case, the patient’s abnormal neck posture, along with physical generals and particular symptoms, were systematically evaluated to monitor treatment progress. The therapeutic outcome demonstrated complete resolution of dystonia, accompanied by overall improvement in various health aspects. A holistic treatment approach, guided by principles of materia medica, organon, and repertory, facilitated individualized case management, contributing to sustained recovery. This case report underscores the efficacy of an integrative approach, wherein a well-indicated single homoeopathic remedy, complemented by customised yoga and meditation techniques, can lead to complete recovery while enhancing the patient’s overall quality of life.
Introduction: Dystonia, classified under ICD code G24.3 [1], is a neurological disorder categorized as a hyperkinetic movement disorder. It is characterized by sustained or intermittent muscle contractions that result in involuntary, repetitive movements, abnormal postures, or both, affecting specific body regions. [2] The global prevalence of cervical dystonia increased from 0.0164% in 2023 to 0.03% in 2024. [3][4] In India, its prevalence in 2023 was 0.0077% among individuals under 30 years but significantly higher at 0.1779% in those aged 50–70 years. [4]
Dystonia is broadly classified into two categories: primary (idiopathic) and secondary (symptomatic). Primary dystonia presents as the sole symptom, occasionally accompanied by tremors or myoclonic jerks involving the dystonic muscles. In contrast, secondary dystonia is associated with other neurological disorders such as Parkinson’s disease, ataxia, ocular motor abnormalities, weakness, spasticity, seizures, or dementia. A genetic component involving DYT genes is observed in some primary dystonia cases, although familial inheritance is rare. Secondary dystonia may arise due to hereditary conditions or external insults. A distinct subcategory of secondary dystonia, known as dystonia-plus syndromes, is hereditary in nature and presents with additional neurological abnormalities without evidence of brain damage. Examples include dopa-responsive dystonia, myoclonus-dystonia, and rapid-onset dystonia-parkinsonism. [5]
Clinically, dystonia is further classified based on the affected body region. Focal dystonia involves a single body region, while segmental dystonia affects two or more contiguous regions. Multifocal dystonia impacts two or more non-contiguous regions, and hemidystonia affects multiple regions on one side of the body. Generalized dystonia involves the trunk and at least two additional body regions. [6]
Cervical dystonia, a form of focal dystonia, affects the cervical muscles, leading to abnormal postures of the head, neck, and shoulders. The movements associated with cervical dystonia occur across different axes: torticollis (head rotation to the left or right along the horizontal axis), retrocollis or anterocollis (backward or forward head flexion along the coronal axis), and laterocollis (head tilting toward the shoulder along the vertical axis). [5]
The condition is marked by key clinical features such as abnormal head, neck, and shoulder movements; neck pain and stiffness; reduced range of motion; spasms; and sensory tricks (geste antagoniste), which patients use to counteract dystonic movements or postures. [5] Additional symptoms include neck pain, occasional mass formation, thickened or tight sternocleidomastoid muscles, cervical spine tenderness, head tremors, asymmetrical shoulder heights, and restricted neck mobility. [4][7]
Diagnosis of cervical dystonia is primarily clinical and relies on physical examination. Patients often exhibit forceful jerks in one direction, followed by slower compensatory movements in the opposite direction. The head is typically tilted to one side, with the chin facing the opposite direction, and the sternocleidomastoid muscle on the affected side appearing prominent, especially when passive correction is attempted. Radiological investigations are usually normal and are conducted primarily to rule out other underlying conditions. [5][8]
The Cervical Dystonia Impact Profile-58 (CDIP-58) is a validated, disease-specific, patient-reported outcome measure developed to evaluate the impact of cervical dystonia on patients’ quality of life. It consists of 58 items grouped into eight domains: head and neck symptoms, pain and discomfort, upper limb activities, walking, sleep, annoyance, mood, and psychosocial functioning. Patients rate each item, with higher scores reflecting greater disease burden or disability. The CDIP-58 has been extensively used in both clinical and research settings to assess treatment outcomes and monitor disease progression. The CDIP-58 demonstrated strong psychometric properties, including reliability, validity, and responsiveness, making it a robust tool for evaluating the multifaceted impact of cervical dystonia.[15][16][17]
Dystonia is a lifelong, painful, and disabling condition. Conventional treatment includes oral medications, intramuscular botulinum toxin injections, and deep brain stimulation; however, these approaches often yield uncertain outcomes. [9] While they may provide immediate relief, they require frequent and increasing dosages, imposing both emotional and financial burdens on patients. In contrast, a holistic treatment approach that integrates individualized homeopathic medicine, personalized movement and breathing exercises, music therapy, and meditation may facilitate comprehensive recovery, promote overall well-being, and contribute to long-term improvement. [10][11][12]
Patient information: A 31-year-old female patient who is an employee in a private company reported a sudden onset dystonia in June 2024. Her neck started tilting to the left side (spasmodic torticollis) and backward (retrocollis).
Initially, she consulted a general physician who prescribed Vitamin D and B12 supplements, but there was no significant improvement. She then visited an orthopaedic specialist, who recommended an MRI, and was subsequently referred to a neurosurgeon. In July, she received a Botox injection, which resulted in a 50% improvement in symptoms. Over time, with the use of a neck belt, her titling improved by 90%, but she continues to experience residual uneasiness, discomfort, neck pain, and right-hand palm pain. There is persistent misalignment in her neck, she can’t keep her head straight. Occasional tremors are present. She also has shoulder pain and back pain, particularly on the right side. The symptoms aggravate on working or doing simple tasks like cooking. Sleeping ameliorates the symptoms.
Previously, the patient suffered from right sided Bell’s palsy in 2020, which resolved within 20 days by physical therapy. She had recurrent abdominal pain since childhood which was triggered by stress. Laparoscopic appendectomy was done in 2008. The patient has occasional bleeding in stools associated with constipation; suspected early-stage piles. Gall bladder polyp was diagnosed but deemed insignificant by the gastroenterologist. Histopathological report done in December 2023 suggested chronic ileitis.
The patient exhibits a deeply sensitive and emotional nature. She has a strong inclination toward peace and harmony and avoids conflicts. Her psychological profile reveals significant emotional vulnerabilities, social insecurities, and stress-induced physical manifestations. She describes herself as “soft-hearted” and highly emotional. She is easily hurt by harsh words and criticism, often leading to episodes of crying. When she feels emotionally overwhelmed, crying and consolation provides her with a sense of relief. She prefers to be surrounded by close family members and a limited social circle, as she feels most comfortable with people who share a similar mindset. The patient has a strong preference for a peaceful environment. She dislikes loud noises, crowded places, and arguments. She does not enjoy parties or loud social gatherings and instead seeks calm and quiet spaces. Her love for nature and meditation further reinforces her need for serenity. In situations where there is excessive noise or conflict, she prefers to leave rather than react aggressively. The patient has a deep emotional connection with her loved ones. She was particularly affected by the death of her grandfather, which left her in a state of shock and speechlessness for hours. She experienced physical manifestations of grief, including cramps in her hands and fainting, requiring medical intervention. This reaction indicates an intense emotional attachment and difficulty processing grief and loss. Additionally, she feels deep sadness and emotional distress over her mother’s chronic illness (rheumatoid arthritis). She constantly worries about her mother’s health and desires to see her recover, which further contributes to her emotional burden.
The patient experiences self-consciousness in social settings due to her cervical dystonia. She fears being judged and observed by others, leading to feelings of insecurity and inferiority. She reports that when people stare at her or inquire about her condition, she feels “different” from others, which causes emotional distress. She avoids situations where she might attract unwanted attention, and this has impacted her confidence and ability to engage freely in social interactions.
The patient has a long history of experiencing physical symptoms in response to stress. She has noted that during stressful situations, particularly in her work life, she develops stomach pain, nausea, and fatigue. This has been a recurring issue since childhood, leading to multiple medical evaluations, including laparoscopic surgery, which revealed no structural abnormalities. She has observed that her symptoms are exacerbated by anxiety, deadlines, and performance pressure.
Her workplace stress stems from the fear of making mistakes, failing to meet deadlines, and the possibility of professional setbacks. She worries about not performing well, falling behind her colleagues, and being reprimanded by superiors. She associates professional failures with a loss of dignity and self-worth, which further heightens her anxiety.
Despite her emotional vulnerabilities, she has developed a strong coping mechanism through meditation. She has been practicing meditation since childhood and has found it beneficial in managing her stress and health concerns. Meditation has helped her reduce the frequency of her stress-induced stomach pain and provides her with a sense of balance and inner peace.
During an exercise where she was asked to create a story from an image, she imagined a woman being chased and attacked while searching for food. When asked to put herself in the woman’s place, she experienced a deep sense of helplessness, rejection, and despair. She described a scenario where she was starving, seeking food, but was met with hostility instead of help. This story suggests underlying fears of rejection, helplessness, and abandonment, possibly linked to past emotional experiences.
She expressed that in moments of distress, she craves solitude and desires to retreat to a peaceful, nature-filled environment, particularly under a tree with shade and fresh air. This indicates her need for emotional security and withdrawal when overwhelmed.
The patient exhibits a good appetite and an adequate thirst, with a preference for cool drinks during summer, indicating a general inclination towards cold. Thermally, the patient is chilly and tends to perspire slightly, primarily on the temples. Sleep is sound, and dreams commonly revolve around daily routine activities. A notable craving is present for mildly sweet foods, particularly brownies. Bowel movements are characterized by constipation, occasionally accompanied by blood staining.
Clinical Findings:
Clinically, the patient presents with a persistent leftward tilt and backward extension of the head (torticollis with retrocollis), accompanied by neck pain, right shoulder discomfort, and occasional tremors. Prominence of the left sternocleidomastoid and posterior cervical muscles is noted on attempted correction. Abnormal posture is constant, while jerky movements are occasional post-Botox. MRI of the cervical spine shows mild reversal of cervical lordosis with focal posterior disc protrusions at C3–C4 and C5–C6 impinging the thecal sac, without nerve root compression. These findings correlate with chronic postural strain but are not the primary cause of dystonia. Neurological examination was otherwise unremarkable.
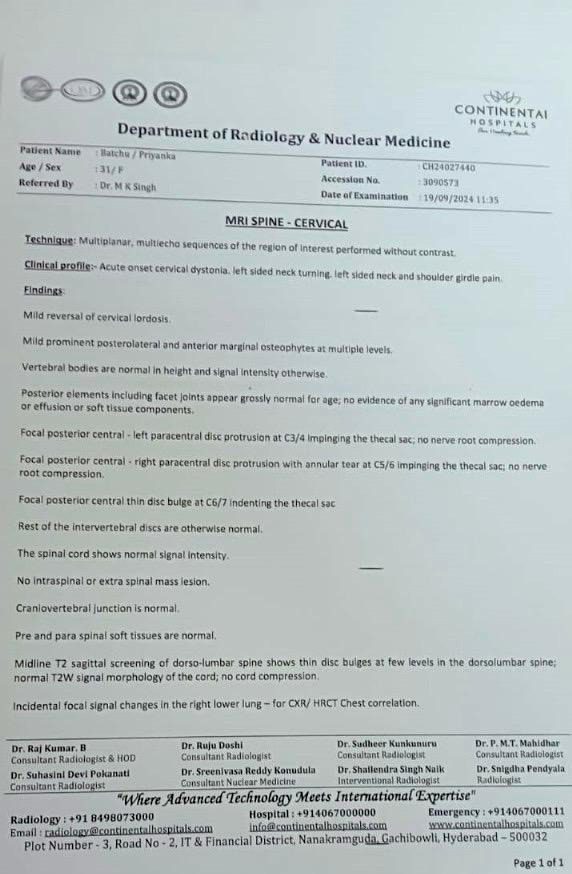
Figure 1: MRI Report page 1
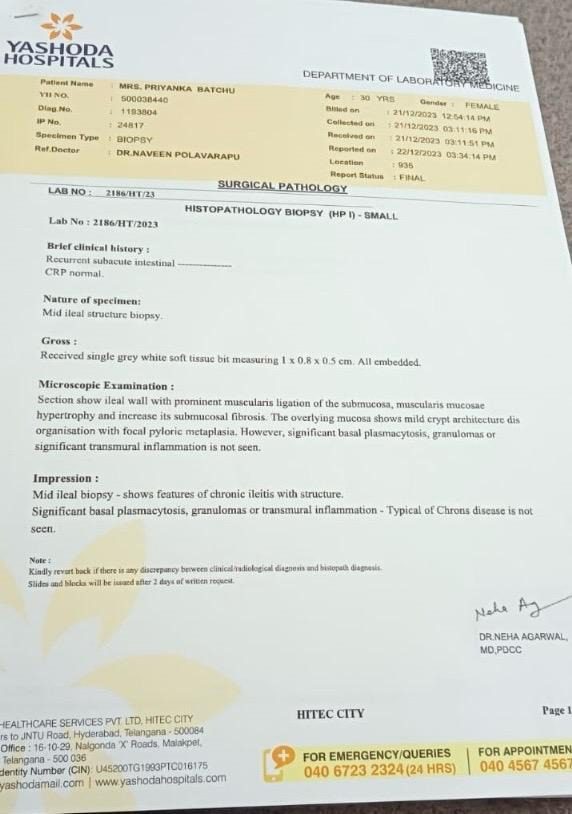
Figure 2: MRI Report page 2
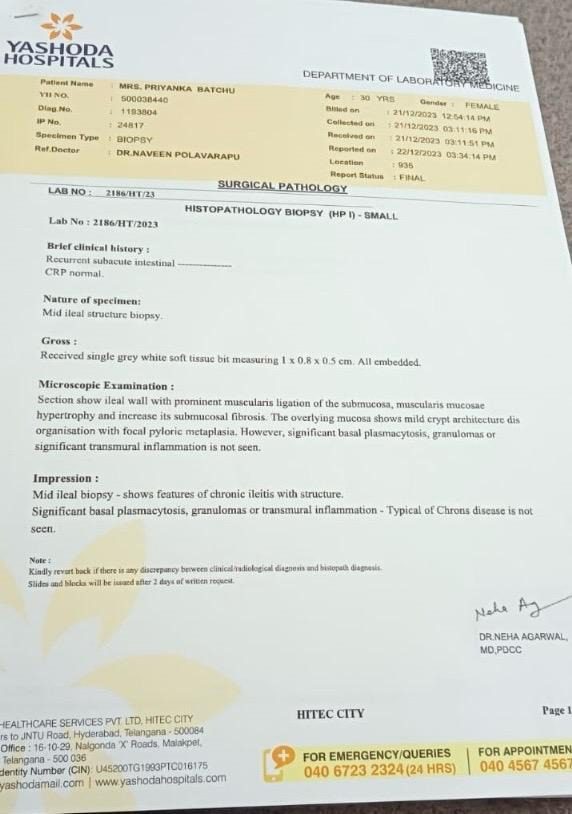
Figure 3: Histopathology Report
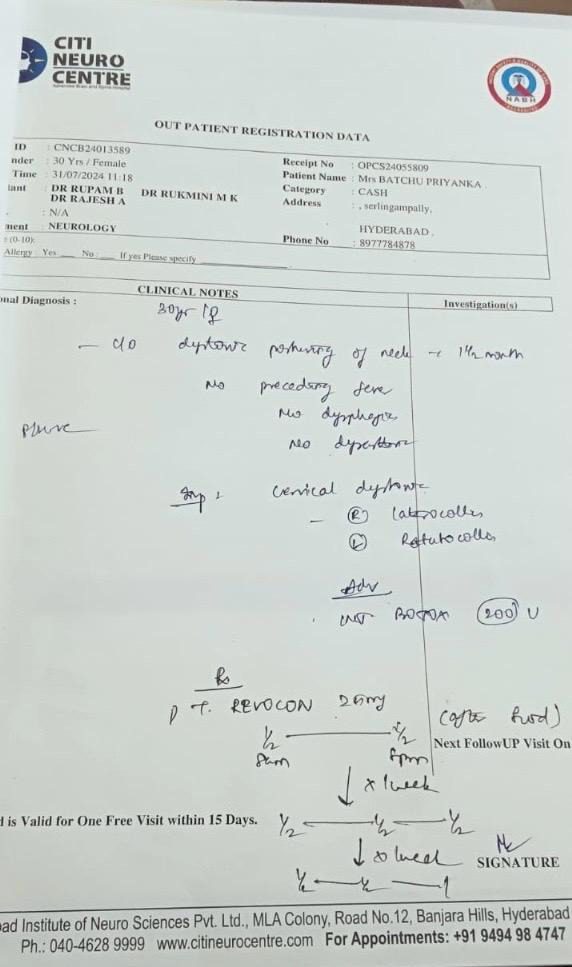
Figure 4: Neurologist prescription
Diagnostic assessment: Diagnosis of dystonia, like other neurological disorders firmly depend upon thorough history taking and complete physical and neurological examination. The head is tilted to one side so that the chin faces to the opposite side. The sterno-mastoid is prominent on the side the head tilts, and becomes more prominent on trying to passively correct the head tilt. Radiological examination is normal, and is carried out to rule out an underlying condition. [5][8] The patient’s tilting had reduced much after Botox treatment but her neck was persistently turned to the left side. The patient was already diagnosed by a neurologist before approaching for homoeopathic treatment.
Therapeutic intervention: The case was assessed through a comprehensive evaluation of the patient’s mental and physical generalities, along with particular symptoms. The patient’s overall response to crisis—characterized by withdrawal, collapse, yielding, and numbness—aligns with the characteristics of the 1st Subclass of Dicotyledons.[13] Therefore, Camphora, as a representative of this subclass, along with its characteristic symptomatology, was identified as the most suitable remedy for this case. Additionally, materia medica literature highlights Camphora‘s well-established action on the cerebrospinal nervous system, further supporting its selection.[14]
Thus, holistic and individualized analysis of the patient’s presentation guided the selection of Camphora as the indicated remedy. The prescribed regimen included Camphora 200, administered twice daily for two days, followed by Camphora 0/6 once daily for one month. Additionally, the patient was advised meditation as it was observed to contribute positively to the condition.
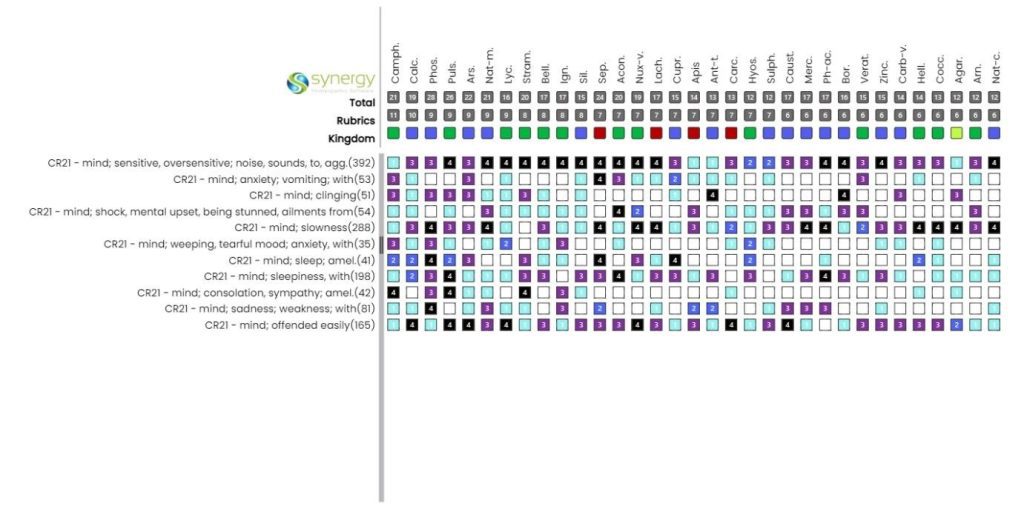
Figure 5: Repertorisation Chart Using Synergy Software
Follow ups and outcomes: The administration of Camphora 200 and Camphora LM 6 led to significant clinical improvements. Notably, the patient’s postural defect was corrected following the initial dose. Symptoms of Bell’s palsy, including tingling and numbness of the right jaw, reappeared after the first prescription but subsequently improved along with pain and occasional tremors following repeated dosing during subsequent follow-ups. At present, the patient is asymptomatic and remains under clinical observation.
Table 1: Follow ups
| DATE | SYMPTOMS | REMARKS | PRESCRIPTION |
| 28/10/24 | Twisting of neck- sometimesNeck misalignment- to the leftNeck Pain- Severe Shoulder pain- Severe Wrist pain- Severe Tremors- OccasionalRight jaw formication & numbness- AbsentAnxiety- SevereStool- ConstipatedSleep- sound | Symptoms of the patient were severe. | Camphora 200, 4 dosesCamphora 0/6 OD for 1 month. |
| 03/12/24 | Twisting of neck- AbsentNeck misalignment- AbsentNeck Pain- AbsentShoulder pain- OccasionalWrist pain- Moderate Tremors- OccasionalRight jaw formication & numbness – MildAnxiety- Moderate Stool- ConstipatedSleep- sound | Current symptoms improved with reappearance of previous symptom suggesting Hering’s law of cure. | SL 4 dosesCamphora 0/6 OD for 1 month. |
| 27/01/25 | Twisting of neck- AbsentNeck misalignment- AbsentNeck Pain- AbsentShoulder pain- AbsentWrist pain- Mild Tremors- AbsentRight jaw formication & numbness – AbsentAnxiety- ReducedStool- BetterSleep- sound | Significant improvement of symptoms | SL 4 doses |
| 01/03/25 | Twisting of neck- AbsentNeck misalignment- AbsentNeck Pain- AbsentShoulder pain- AbsentWrist pain- AbTremors- AbsentRight jaw formication & numbness – AbsentAnxiety- ReducedStool- BetterSleep- sound | No complaints | SL 4 doses |
The patient’s progress was assessed using the CDIP-58scale, with the total score reducing from 45.6% to 2.1% over a period of three months. [15][16][17]
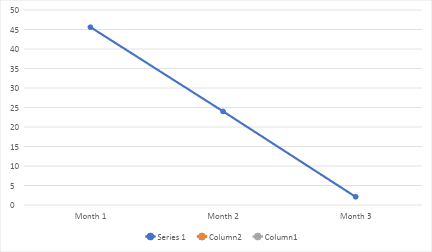
Figure 6: CDIP-58 (in percentage)
Discussion: Dystonia, particularly cervical dystonia, poses significant challenges in clinical management due to its multifactorial aetiology and heterogeneous response to conventional therapies. In this case, despite undergoing botulinum toxin treatment, the patient experienced only partial relief, with persistent residual symptoms continuing to affect her quality of life.
Holistic medicine recognizes that disease manifestations are not isolated phenomena but rather reflections of an underlying imbalance in the individual’s overall health. Holism, in the Organon of Medicine written by German physician Dr. Samuel Hahnemann, is not just about treating symptoms but understanding the patient as a complete entity—mind, body, and spirit. [18] Homoeopathy, founded on the principle of individualized treatment, provides a holistic therapeutic approach by addressing not only the physical pathology but also the mental, emotional, and constitutional aspects of the patient. By restoring balance to the vital force, Homoeopathy aims to achieve deep and lasting healing.
In the given case, a detailed case analysis identified the basic nature of patient as sensitive for the surrounding and as withdrawal in crisis situations. This gives indication for the medicine from 1st Subclass of dicotyledons of plant kingdom.[13] Exact member from this large group is identified by characteristic and peculiar symptoms of the case through repertorization and materia medica confirmation. After carefully analysing all these aspects, Camphora is the most appropriate remedy, aligning with the patient’s complete symptomatology (refer figure 1). The administration of Camphora 200, followed by Camphora 0/6, resulted in marked symptomatic relief, evidenced by the resolution of dystonic postures, significant pain reduction, and an overall enhancement in well-being.
The follow-up assessments demonstrated progressive recovery in accordance with Hering’s Law of Cure, wherein older symptoms temporarily resurfaced before subsiding, suggesting a deep, curative response rather than mere symptomatic palliation. Notably, the patient’s emotional health improved, with reductions in anxiety and enhanced coping mechanisms, further reinforcing the holistic impact of individualized homoeopathic intervention.
A pivotal aspect of this case was the integration of supportive therapies, including meditation and lifestyle modifications, alongside homoeopathic treatment. Meditation, recognized for its neuromodulatory effects and stress-reducing properties, likely contributed to the overall therapeutic outcome by addressing stress-induced exacerbations of dystonia. The substantial decline in the Cervical Dystonia Impact Profile (CDIP-58) score from 45.6% to 2.1% over three months provides objective evidence of the effectiveness of this integrative approach.
This case emphasizes the efficacy of a holistic, patient-centred approach in the management of dystonia, demonstrating the synergistic interaction between homoeopathy and supportive therapies in promoting comprehensive recovery.
Conclusion:
This case report illustrates the potential of an individualized, holistic homoeopathic approach in promoting significant recovery from dystonia. The patient, previously unresponsive to conventional treatment, improved markedly with Camphora and supportive interventions. This outcome highlights the interconnectedness of physical and psychological health, reinforcing the role of the PNEI axis in both pathogenesis and healing. Homoeopathy, when tailored to the individual, offers a non-invasive, cost-effective, and patient-centred option for managing movement disorders. Further clinical studies and well-structured research trials are essential to substantiate these observations and expand the role of homoeopathy in the integrative management of movement disorders.
Declaration of patient’s consent: A written informed consent was taken from the patient, and he was assured of anonymity while reporting his case.
Financial support and sponsorship: Nil
Conflicts of interest: There are no conflicts of interest.
References:
1. ICD-10-CM code for dystonia [Internet]. Available from: https://www.icd10data.com/ICD10CM/Codes/G00-G99/G20-G26/G24-
2. Neychev VK, Fan X, Mitev V, Hess EJ, Jinnah HA. Dystonia: A review. Semin Neurol [Internet]. 2018 [cited YYYY MM DD];66(1):9. Available from: https://journals.lww.com/neur/fulltext/2018/66001/dystonia__a_review.9.aspx
3. Stephen CD, Dy-Hollins M, Melo C, Al Qahtani X, Sharma N. Dystonias: Clinical recognition and the role of additional diagnostic testing. Semin Neurol. 2023 Mar;43:1-12.
4. Cervical dystonia: Etiology, clinical features, and diagnosis [Internet]. UpToDate. Available from: https://www.uptodate.com/contents/cervical-dystonia-etiology-clinical-features-and-diagnosis/print
5. Warner TT, Bressman SB, editors. Clinical diagnosis and management of dystonia. 1st ed. London: Informa Healthcare; 2007.
6. National Library of Medicine [Internet]. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10226676/
7. Torticollis: MedlinePlus medical encyclopedia [Internet]. MedlinePlus. Available from: https://medlineplus.gov/ency/article/000749.htm
8. Maheshwari J, Mhaskar VA. Essential orthopaedics: Including clinical methods. New Delhi: Jaypee Brothers Medical Publishers; 2019.
9. Snaith A, Wade D. Dystonia. BMJ Clin Evid [Internet]. 2014. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3938056/
10. Xue SA, de Schepper L, Hao GJ. Treatment of spasmodic dysphonia with homeopathic medicine: A clinical case report. Homeopathy. 2009;98(1):56-9.
11. Using the brain to retrain the body to overcome dystonia [Internet]. The Globe and Mail. Available from: https://www.theglobeandmail.com/life/health-and-fitness/health/using-the-brain-to-retrain-the-body-to-overcome-dystonia/article23342529/
12. Runner’s dystonia: The mysterious malady that causes mind and muscle to lose touch [Internet]. Runner’s World. Available from: https://www.runnersworld.com/health-injuries/a20865203/runners-dystonia-mysterious-malady-causes-mind-and-muscle-to-lose-touch/
13. Sankaran R. Superclass in homoeopathy. Mumbai: Homoeopathic Medical Publishers.
14. Phatak SR. The concise materia medica. New Delhi: B. Jain Publishers.
15. Cano SJ, Hobart JC, Edwards M, Fitzpatrick R, Bhatia K, Thompson AJ, et al. CDIP-58 can measure the impact of botulinum toxin treatment in cervical dystonia. Neurology. 2006;67(12):2230-2.
16. Cano SJ, Warner TT, Linacre JM, Bhatia KP, Thompson AJ, Fitzpatrick R, et al. Capturing the true burden of dystonia on patients: The Cervical Dystonia Impact Profile (CDIP-58). Neurology. 2004;63(9):1629-33.
17. Cano SJ, Warner TT, Thompson AJ, Bhatia KP, Fitzpatrick R, Hobart JC. The Cervical Dystonia Impact Profile (CDIP-58): Can a Rasch-developed patient-reported outcome measure satisfy traditional psychometric criteria? Health Qual Life Outcomes. 2008;6(1):58.
18. Hahnemann S. Organon of medicine. 6th ed. New Delhi: B. Jain Publishers.
15- 9. Cano SJ, Warner TT, Thompson AJ, Bhatia KP, Fitzpatrick R, Hobart JC. The Cervical Dystonia Impact Profile (CDIP-58): Can a Rasch-developed patient-reported outcome measure satisfy traditional psychometric criteria? Health Qual Life Outcomes. 2008 Aug 6;6:58. doi: 10.1186/1477-7525-6-58. PMID: 18684327; PMCID: PMC2538506
16- 10. Cano SJ, Warner TT, Linacre JM, Bhatia KP, Thompson AJ, Fitzpatrick R, Hobart JC. Capturing the true burden of dystonia on patients: The Cervical Dystonia Impact Profile (CDIP-58). Neurology. 2004 Nov 9;63(9):1629–33. doi:10.1212/01.WNL.0000142962.11881.26. PMID:15534247.
17- 11. Cano SJ, Warner TT, Linacre JM, Bhatia KP, Thompson AJ, Fitzpatrick R, Hobart JC. Capturing the true burden of dystonia on patients: The Cervical Dystonia Impact Profile (CDIP-58). Neurology. 2004 Nov 9;63(9):1629–33. doi:10.1212/01.WNL.0000142962.11881.26. PMID:15534247.
9- 12. Snaith A, Wade D. Dystonia. BMJ Clin Evid [Internet]. 2014 Feb 28 [cited 2025 Jul 30];2014:1211. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3938056/
10- 13. Xue SA, de Schepper L, Hao GJ. Treatment of spasmodic dysphonia with homeopathic medicine: a clinical case report. Homeopathy. 2009 Jan;98(1):56–9. doi:10.1016/j.homp.2008.11.004. PMID: 19135961.
11- 14. Leung W. Using the brain to retrain the body to overcome dystonia. The Globe and Mail [Internet]. Last update Jan 2016 [cited 2025 Jul 30]. Available from: https://www.theglobeandmail.com/life/health-and-fitness/health/using-the-brain-to-retrain-the-body-to-overcome-dystonia/article23342529/
12- 15. Kuzma C. Runner’s dystonia: The mysterious malady that causes mind and muscle to lose touch. Runner’s World [Internet]. 2019 Jun [cited 2025 Jul 30]; Available from: https://www.runnersworld.com/health-injuries/a20865203/runners-dystonia-mysterious-malady-causes-mind-and-muscle-to-lose-touch/
13- 16. Sankaran R. Superclass in homoeopathy. Mumbai: Homoeopathic Medical Publishers;2023
14- 17. Phatak SR. Materia Medica of Homoeopathic Medicines. 3rd ed. New Delhi: B. Jain Publishers; 2005.
About the Author:
Dr. Kamlesh Kakde
About the Co-Author:
Dr. Vinaya Iyer, BHMS, MD (Hom.)