ABSTRACT
Vulvovaginitis is an inflammation or infection of the vulva and vagina. It’s a common condition that affects women and girls of all ages. Vulvovaginitis is a common day to day problem in gynecological practice. Candida albicans is the commonest infectious cause. An estimated 75% of women have at least one episode of Vulvovaginal candidiasis, and 40%–45% will have two or more episodes within their lifetime. Its rate is 30-45% in women
KEYWORDS : Vulvovaginitis, Caladium
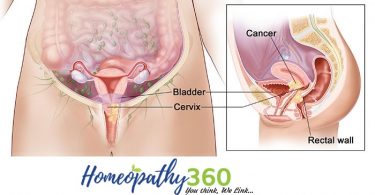
INTRODUCTION: Vaginitis is an inflammation of the mucous membranes of the vagina. It may be caused by a viral, bacterial, trichomonas, or yeast infection, or by sexual intercourse, douching, or other irritants such as spermicides, chemicals, or a foreign body in the vagina. Atrophic vaginitis occurs in women past menopause, resulting from a decrease in estrogen levels.
Bacterial vaginosis and genital Candida infection were present in almost a quarter of patients. This prevalence’s were similar to those reported in other studies involving adolescents in Brazil and other countries. In our study, the rate of Trichomonas vaginalis infection was low, about 1%. In Brazil, the prevalence of T. vaginalis was 3.2% in women aged from 18 to 40 years followed at a primary care health service. The literature unveils great variability in the prevalence rates of trichomoniasis, that may be due to heterogeneity regarding the diagnostic methods used and the group evaluated. Despite its clinical applicability, vaginal cytology has lower sensitivity and specificity rates for diagnosing T. vaginalis when compared to parasitological and molecular diagnosis, such as direct microscopy, the culture, and polymerase chain reaction. Sutton et al., using molecular techniques, reported a prevalence of 2.1% in a population of 1416 adolescents aged 14–19 years from non-Hispanic white, non-Hispanic black, and Mexican-American ethnicity. On the other hand, Krashin et al. and Crosby et al., also in the United States, reported higher prevalence rates, 12.9% and 14.4%, respectively. Both studies used culture methods to detect T. vaginalis and were carried out among socioeconomically disadvantaged adolescents, mostly nonwhite patients, that attended public outpatient clinics, similar to the ones included in our study. However, the individuals included in these studies reported a high frequency of sexual intercourse with non-steady, older partners, significant history of delinquency and illegal drug use, and concurrent Neisseria gonorrhoeae infection, characteristics that differentiate these adolescents from our population.1
The presence of bacterial vaginosis was
associated with multiple sexual partners (P = 0.01).
In spite of the fact that bacterial vaginosis is not considered an STD, a greater
risk for being diagnosed with this disease has been identified in patients with
multiple sexual partners, which is
consistent with our study. In this sense, due to the number of sexual partners,
in association with the commonly
described irregular condom use among this population, one could infer that these adolescents were likely at increased risk for other STDs.
The use of alcohol, tobacco, and illegal drugs was found be associated with bacterial vaginosis. However, it should be interpreted as an indirect risk factor for bacterial vaginosis, since the use of these substances is usually related to practices such as irregular condoms use and poor genital hygiene, that foster the development of this condition. Genital infection by Candida albicans was not associated with any of the risk factors evaluated, although some studies have reported that oral sex and sexual activity are important risk factors for genital infection by this microorganism.
Vulvovaginitis is an important public health problem, not only due to the gynecological and obstetric complications associated with it but also because the inflammation of the vaginal mucosa and the reduction of lactobacilli could facilitate the transmission of STDs, especially HIV infection. Moreover, the studied population showed a low frequency of condom use and a high number of sexual partners, behaviours that could lead to an important increase in the risk for STDs among these adolescents2.
Infection is the most common cause of vaginitis ,including candidiasis, bacterial vaginosis, and trichomoniasis. After puberty, infectious vaginitis accounts for 90 percent of cases.
Less commonly, vaginitis may also be caused by gonnorrhea, Chlamydia, mycoplasma, herpes, campylobacter, some parasites, and poor hygiene.
Vaginitis can occur before puberty, but different types of bacteria may be involved. Before puberty, Streptococcus is a more likely cause, sometimes because improper hygiene practices spread bacteria from the anal area to the genitals.
The proximity of the vagina to the anus, lack of estrogen, lack of pubic hair, and lack of labial fat pads may increase the risk of vulvovaginitis in before puberty. Vulvovaginitis is an inflammation of the vagina and vulva. It can affect women of all ages.
After puberty, infection is most often due to Gardnerella.
Sometimes, vaginitis can stem from an allergic reaction, for example, to condoms, spermicides, certain soaps and perfumes, douches, topical medications, lubricants, and even semen.
Irritation from a tampon can also cause vaginitis in some women. Factors that increase the risk of vaginitis include:
- pregnancy
- douching and using vaginal products, such as sprays, spermicides, and birth control devices
- using antibiotics
- wearing tight pants or damp underwear
- low estrogen levels during menopause
Women with diabetes are particularly prone to vaginitis.
Vulvovaginal infections mainly occur as vulvovaginitis. A few are sexually transmitted (STI), but others are not. In non-sexually transmitted vulvovaginitis, the infectious agent can be a commensal, opportunistic or exogenous microorganism. Vulvovaginitis due to Candida Albicans (C. albicans) or other Candida can affect up to 75% of women at least once in their lifetime. Bacterial vaginosis due to a very different infectious agent like (Gardenerellavaginalis (G. vaginalis), Prevotellasp, Bacteroidessp, Mobiluncussp, Mycoplasma hominis (M. hominis) and Ureaplasmaurealyticum (U. urealyticum)) is by far the most common cause of vaginal discharge in childbearing women. Vaginitis secondary to STIs, are the consequence of cervical infections. It is most often the following sexually transmitted germs: Trichomonasvaginalis (T. vaginalis), Neisseria gonorrheae (N. gonorrheae), Chlamydia trachomatis (C. trachomatis) and Mycoplasma genitalium (M. genitalium). Herpes virus 1 and 2 are other sexually transmitted infections which can cause vulvovaginitis. Human papillomavirus (HPV) serotypes 6 and 11 are the cause of condylomas in 70 to 100% of cases. STIs are a public health problem in industrialized countries and especially in developing countries. The serious gyneco-obstetric and neonatal complications they cause make their prevention and management particularly important. In Senegal, to our knowledge, there is no studies of the etiologies of vulvovaginitis in dermatology department.3
The most common symptoms of vaginitis include:
- irritation of the genital area
- discharge that may be white, grey, watery, or foamy
- inflammation, leading to redness and swelling of the labia majora, labia minora, and perineal area, mainly due to an excess of immune cells
- dysuria, which is pain or discomfort when urinating
- painful sexual intercourse, known as dyspareunia
- foul or fishy vaginal odour.
Prevention
The following best practices may help prevent vaginitis:
- Having good overall hygiene
- Using mild soaps without irritants or scents
- Wearing cotton underwear
- Avoiding douching and irritating agents, such as those present in hygiene sprays, soaps, and other feminine products
- Wiping from front to back to avoid spreading bacteria from the anus to the vagina
- Wearing loose-fitting clothing
- Practicing sex with a condom using antibiotics only when necessary.
- Keep your genital area clean and dry when you have vaginitis.
- Avoid soap. Just rinse with water to clean yourself.
- Soak in a warm, not hot, bath to help your symptoms. Dry thoroughly afterward.
Avoid douching. Many women feel cleaner when they douche, but it may actually make symptoms worse because it removes healthy bacteria that line the vagina. These bacteria help protect against infection.6
Other tips are:
- Avoid using hygiene sprays, fragrances, or powders in the genital area.
- Use pads instead of tampons while you have an infection.
- If you have diabetes, keep your blood sugar level in good control. Allow more air to reach your genital area. You can do this by:
- Wearing loose-fitting clothes and not wearing panty hose.
- Wearing cotton underwear (instead of synthetic fabrics) or underwear that has a cotton lining in the crotch. Cotton allows normal evaporation of moisture so that moisture buildup is reduced.
- Not wearing underwear at night when you sleep. Girls and women should also:
- Know how to properly clean their genital area while bathing or showering.
- Wipe properly after using the toilet. Always wipe from front to back.
- Wash thoroughly before and after using the toilet.4
HOMOEOPATHIC APPROACH
CALADIUM SEGUINUM
American arum
Tincture of whole fresh plant
The leaves of the caladium has more alkaloid than the bulbs, stem and roots. Alkaloids have been used as CNS stimulant, topical anesthetic in ophthalmology, powerful pain relievers and antiupuretic action. This remedy has a marked action on the genital organs, and pruritus of this region. 5
CLINICAL – IRRITATION, PRURITUS VAGINA
CHARECTERISTICS
- Like the other Arums,
caladium has an intensely irritating effect on the mucous membranes
and skin and produces many burning sensations.
- it is one of the best remedies for that troublesome affection, pruritus vulva.
- Itching of vulva with burning.
- There is aggravation from warmth; aversion to cold water, but bathing with cold water >>itching
- All symptoms >> after sweat; after sleeping in the daytime.
- Motion agg. most symptoms.6
FEMALE SEXUAL ORGANS
- This remedy has a marked action
on the genital organs and pruritus of this region.
- pruritus of vulva and vagina during pregnancy.7
- Itching of external genitals with voluptuousness
- Cramp pain in uterus at night
- Burning sensation and erysipelatous inflammation
Modalities – better after sweat,after sleeping in daytime worse – motion.6
Caladium seguinum treatment for Female ailments: Pruritus of vulva (Ambr; Kreos) and vagina during pregnancy (Hydrogen peroxyd 1: 12 locally). Voluptuousness. Cramp pains in uterus at night.5
REFERENCE
1.Candidial vulvovaginitis Jack D Sobel, Clinical obstetrics and gynecology 36(1),153-165,1993 2.Acute vulvovaginitis Linda O Eckert .New Engaland journal of medicine 355 (12),1244-1252 , 2006
- Vulvovaginitis in pubertal girls T stricker ,F Navratil ,FH Sennhauser ,Archives of disease in childhood 88(4),324-326 ,2003
- Risk factors for candida vulvovaginitis, BARBARA D Reed, Obsterical and gynecological survey 47 (8),551 -560,1992
- Acharya AK. Caladium cultivation: for ornamental, medicine and export.Pg 11 – 12
- Boericke, W., 2007. Boericke’s new manual of homoeopathic materia medica with repertory. New Delhi:
B. Jain Publishers.
- Clarke, J., 1996. A Dictionary of Practical Materia Medica In Three Volumes (Volume III). Delhi, India: B. Jain Publisheres;vol 1
ABOUT AUTHOR
DR LAKSHMIPRIYA.B.MENON
FATHER MULLER HOMOEOPATHIC MEDICAL COLLEGE AND HOSPITAL