BEDWETTING: Know your child; some non-medicinal managements.
ABSTRACT:
Bedwetting is a commonly encountered clinical condition. Before you get worried about your child, there are some normal milestones that you need to know. Apart from this, if the child is still having bed wetting, there are some non-medicinal aspects that you can try. Children develop normal micturition reflex by the age of 2 to 2.5 years. This period varies from child to child. To control bed-wetting, strategies like restricting water intake after 8 PM are greatly helpful.
KEY WORDS:
Bed wetting. Normal milestones. Non- medicinal management. Parent-child relationship.
INTRODUCTION:
Enuresis is the repeated voiding of urine into clothes or beds, whether the voiding is involuntary or intentional. The behavior must occur twice weekly for at least 3 months or must cause clinically significant distress or impairment socially or academically. The child’s chronological or developmental age must be at least 5 years. (1)
So, by definition, it is clear that we will not label any child enuretic before 5 years and without proper repetition of the event.
NORMAL TIMELINE OF DEVELOPMENT OF BLADDER REFLEX:
| AGE | NORMAL BEHAVIOR |
| First 8 months | A child voids urine as soon as he/she eats something. |
| 15- 18 months | Voluntary control over the bladder starts, but no time to ‘catch’. (urgency phase). |
| 18- 24 months | The child tells the mother sufficient time before. |
| After 24 months | Able to pull his/ her pants down & go to the lavatory. |
Table 1: NORMAL TIMELINE OF DEVELOPMENT OF BLADDER REFLEX. (2)
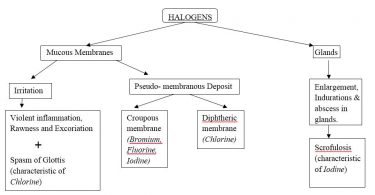
CAUSES OF ENURESIS:
Causes of enuresis are generally divided into 2 broad classes: Organic and Non-Organic (1).
Organic causes are further divided into the following sub-types:
Figure 1 Organic causes of bed wetting.
The organic type of nocturnal enuresis requires strict management as per the cause and presentation of the disease.
Once we rule out the organic causes, there are many non-organic causes also. They are described as below:
Figure 2 non-organic causes of Bed wetting (2).
- CONDITIONING DEFECT: if the child is punished for not using a pottie when placed, he will become conditioned against it and may refuse to use it.
- LEARNING DEFECT: if the child is negatively reinforced in his/ her developmental period for not using the toilet, those children tend to be enuretic.
- HINMAN’S SYNDROME: When a child intentionally holds urine for a longer period and afterwards there comes a point in which urine passes involuntarily.
- PSYCHOLOGICAL STRESSOR: Bedwetting can be due to reflex action of some psychological stressor through which the child is passing through e.g. fright, fights of parents, night terrors, jealousy, domestic friction, etc.
- GENETIC FACTORS: children whose at least one parent is enuretic, have a higher risk of being enuretic.
- SOCIO ECONOMIC CONDITIONS: Socioeconomic conditions of parents can influence widely upon the enuretic behavior of children.
- PERSONALITY OF MOTHER: A mother who is determined to teach discipline early, is the mother who is likely to meet with refusal to use the pottie.
- DEPTH OF SLEEP: Bed-wetters are heavy sleepers.
When enuresis is caused by such non-organic causes, we can manage it by non-medicinal approaches (3).
NON-MEDICINAL PART OF MANAGEMENT OF BED WETTING.
Management consists of one or more of the following measures (3):
- Restriction of fluid intake after 8 PM, in nocturnal enuresis.
- Bladder training during the daytime is aimed at increasing the holding time of the bladder. This is carried out in a step-by-step manner using positive reinforcements.
- Interruption of sleep before the expected time of bed wetting. The child should be fully woken up and made aware of the passing of urine.
- Conditioning devices: cause an alarm to sound as soon as the voided urine touches the bed sheet. It is important to check the child’s hearing before starting treatment. The alarm causes inhibition of further micturition and the child awakens. If properly used, it is an effective method of therapy.
- Supportive psychotherapy for the child, parents and the whole family is often needed.
CONCLUSION:
Bedwetting can be caused by various factors. An effective and supportive parent-child relationship is a prime requirement for gaining control over the problem. The role of caregivers should not be neglected during the treatment. Support for children is the key to overcoming the problem.
References
| 1. | Sadock BJ, Sadock VA. KAPLAN & SADOCK’S Concise Textbook of Child and Adolescent Psychiatry Philadelphia: LIPPINCOIT WILLIAMS & WILKINS, a WOLTERS KLUWER BUSINESS; 2009. |
| 2. | Master FJ. Bed wetting Enuresis. 9th ed. Noida: B. Jain Publishers (P) LTD.; 2016. |
| 3. | Ahuja N. A short textbook of Psychiatry New Delhi: Jaypee Brothers Medical Publishers (P) ltd; 2023. |