INTRODUCTION-
Acute kidney injury (AKI), previously referred to as acute renal failure, is not a diagnosis; rather it describes the situation where there is a sudden and often reversible loss of renal function, which develops over days or weeks and is often accompanied by a reduction in urine volume. Approximately 7% of all hospitalised patients and 20% of acutely ill patients develop AKI. In uncomplicated AKI mortality is low, even when RRT is required. In AKI associated with sepsis and multiple organ failure, mortality is 50–70% and the outcome is usually determined by the severity of the underlying disorder and other complications, rather than by kidney injury itself. Elderly patients are at higher risk of developing AKI and have a worse outcome.
PATHOPHYSIOLOGY-
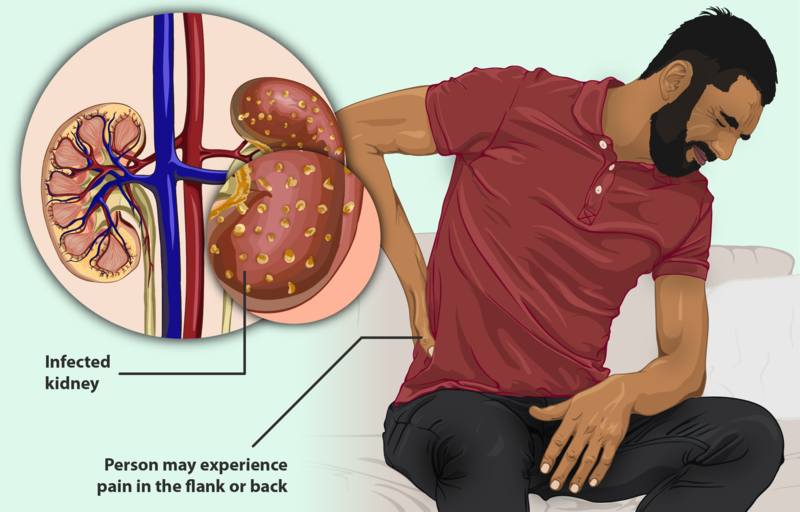
There are many causes of AKI and it is frequently multifactorial.It is helpful to classify it into three subtypes:
• ‘pre-renal’, when perfusion to the kidney is reduced
• ‘renal’, when the primary insult affects the kidney itself
• ‘post-renal’, when there is obstruction to urine flow at any point from the tubule to the urethra .
In pre-renal AKI, a reduction in perfusion reduces GFR. If the result is not corrected, this may lead to ‘renal’ injury: namely, acute tubular necrosis (ATN). Histologically, the kidney shows inflammatory changes, focal breaks in the tubular basement membrane and interstitial edema.Dead tubular cells may also be shed into the tubular lumen,leading to tubular obstruction.
Renal AKI may be caused by nephrotoxic drugs , which can cause ATN or allergic interstitial nephritis. The other common ‘renal’ cause is glomerulonephritis, in which there is direct inflammatory damage to the glomeruli .
Post-renal AKI occurs as the result of obstruction to the renal tract. This leads to elevation of intraluminal ureteral pressure transmitted to the nephrons after prolonged obstruction, with a subsequent fall in GFR. If the obstruction is not relieved,the low GFR is maintained by a drop in renal blood flow rate via thromboxane A2 and angiotensin II.
ETIOLOGY-
PRE-RENAL
Impaired perfusion:
- Cardiac failure
- Sepsis
- Blood loss
- Dehydration
- Vascular occlusion
RENAL
Glomerulonephritis
Small-vessel vasculitis
Acute tubular necrosis
• Drugs
• Toxins
• Prolonged hypotension
Interstitial nephritis
• Drugs
• Toxins
• Inflammatory disease
• Infection
POST-RENAL
- Urinary calculi (bilateral)
- Retroperitoneal fibrosis
- Benign prostatic
- enlargement
- Bladder cancer
- Prostate cancer
- Cervical cancer
- Urethral stricture/valves
CLINICAL FEATURES-
Signs and symptoms of acute kidney failure may include:
- Decreased urine output, although occasionally urine output remains normal
- Fluid retention, causing swelling in your legs, ankles or feet
- Drowsiness
- Shortness of breath
- Fatigue
- Confusion
- Nausea
- Seizures or coma in severe cases
- Chest pain or pressure
Sometimes acute kidney failure causes no signs or symptoms and is detected through lab tests done for another reason.
INVESTIGATIONS–
If your signs and symptoms suggest that you have acute kidney failure, your doctor may recommend certain tests and procedures to verify your diagnosis. These may include:
- Glomerular filtration rate (GFR) – GFR is a test that measures the glomerular filtration rate – it compares the levels of waste products in the patient’s blood and urine. GFR measures how many milliliters of waste the kidneys can filter per minute. The kidneys of healthy individuals can typically filter over 90 ml per minute.
- Urine tests. Analyzing a sample of your urine, a procedure called urinalysis, may reveal abnormalities that suggest kidney failure.
- Blood tests. A sample of your blood may reveal rapidly rising levels of urea and creatinine – two substances used to measure kidney function.
- Imaging tests. Imaging tests such as ultrasound and computerized tomography may be used to help your doctor see your kidneys.
- Kidney biopsy-Small sample of kidney tissue is extracted and examined for cell damage. An analysis of kidney tissue makes it easier to make a precise diagnosis of kidney disease.
MANAGEMENT OF ACUTE KIDNEY INJURY-
- Assess fluid status as this will determine fluid prescription If hypovolaemic: optimise systemic haemodynamic status with fluid challenge and inotropic drugs if necessary .Once euvolaemic, match fluid intake to urine output plus an additional 500 mL to cover insensible losses If fluid-overloaded, prescribe diuretics (loop diuretics at high dose will often be required); if the response is unsatisfactory, dialysis may be required.
- Administer calcium resonium to stabilise myocardium and glucose
- and insulin to correct hyperkalaemia if K+ > 6.5 mmol/L as a holding measure until a definitive method of removing potassium is achieved (dialysis or restoration of renal function).
- Consider administering sodium bicarbonate (100 mmol) to correct acidosis if H+ is > 100 nmol/L (pH < 7.0).
- Discontinue potentially nephrotoxic drugs and reduce doses of therapeutic drugs according to level of renal function.
- Ensure adequate nutritional support.
- Consider proton pump inhibitors to reduce the risk of upper gastrointestinal bleeding
- Screen for intercurrent infections and treat promptly if present.
- In case of urinary tract obstruction, drain lower or upper urinary tract as necessary
HOMOEOPATHIC REMEDIES-
- Arsenicum Album- Arsenic album is an effective remedy for renal failure with high level of creatinine in blood. Urine is scanty, burning when urinating. Albuminuria. Epithelial cells, cylindrical clots of fibrin and globules of pus and blood in urine. Feeling weakness in abdomen after urination. Retention of urine.Urine black as if mixed with dung.
- Aralia Hispida -Aralia hispida is found to be effective for high level of creatinine in blood. There is dropsy of renal origin. Urinary tract infection is present. Urine is scanty leading to complete suppression of urine. Renal diseases with constipation.
- Apis Mellifica – Apis mel is another effective remedy where edematous swellings of face and extremities are present with thirstlessness. Urination frequent but scanty. There is a feeling of suffocation and breathing difficult. All symptoms are worsen from heat and better from cold.
- Belladonna – Belladonna is used in the acute stage where uremia occurs in healthy patients when kidney ceases to function and urine becomes dark and turbid. There is twitching of the muscles with violent convulsions.
- Cuprum Aceticum – In Cuprum aceticum the tongue is pale , coated with lot of mucus. Anemia. Pulse rapid. The patient is chilly. Breathlessness with dry cough. Cannot eat or drink without retching.
- Cuprum Arsenitum –Cuprum ars is also a very effective remedy for Renal failure with high level of creatinine in blood. There is kidney inefficiency and uremia. The urine smell like garlic. Urine of high specific gravity increased, acetones and diacetic acid.
- Helleborus Niger – Hellebotus is best for high creatinine in blood with remia and unconsciousness. Pupils dilated and insensible to light. Convulsion is present. The body have a strong urinous odor.
- Lycopodium Clavatum —Lycopodium is an effective remedy for high level of creatinine in blood. Urine scanty , cries before urinating, red sand in urine, must strain, suppressed or retained. Urine milky and turbid. Sometimes haematuria . Urine is burning and hot. The right kidney is mainly affected. The patient experiences impotency.The patient likes warm food and drink, also there is intense craving for sweets.
- Mercurius Corrosivus —Merc cor is effective for acute renal failure with albuminous urine, which is scanty , hot, burning ,passed drop by drop or suppressed , bloody, greenish discharge.Tenesmus of bladder. There is stabbing pain extending up urethra into bladder.There are severe lumbar pain and dyspnoea.
- Urtica urens —Useful in cases when there is high serum uric acid levals; gouty & rheumatic diathesis; Worse, from snow-air; water, cool moist air, touch.
REFERENCES-
- Penman, Ian D., et al., editors. Davidson’s Principles and Practice of Medicine. 23th ed., Elsevier Health Sciences, 2018.
- Boericke W. New Manual of Homoeopathic Materia Medica and Repertory. Reprint Edition New Delhi: B. Jain Publishers(P)Ltd.; 2011.
ABOUT AUTHOR-
Dr. Rahul Kumar Mehra MD Scholar (Homoeopathic Pharmacy) Batch- 2020-2021
- HOD- Dr. Chetna Pandey
- Guide- Dr. Hemant Kumar Soni
Government Homoeopathic Medical College & Hospital, Bhopal. M.P