ABSTRACT
The study of different articles, textbooks of medicine and dermatology especially revealed that acne vulgaris is one of the most common inflammatory skin troubles characterised by several skin lesions including clinicopathological changes such as comedones, papules, pustules , nodules, cystic lesions leading to ultimate result of scar formation. Acne affects skin having dense sebaceous follicles in areas including face, chest and back. Acne is not life threatening but severe acne can affect psychological status and social activities. The present review focuses on an epidemiology, etiology, pathogenesis, diagnosis, differential diagnosis and management of acne with homoeopathic medicine.
INTRODUCTION
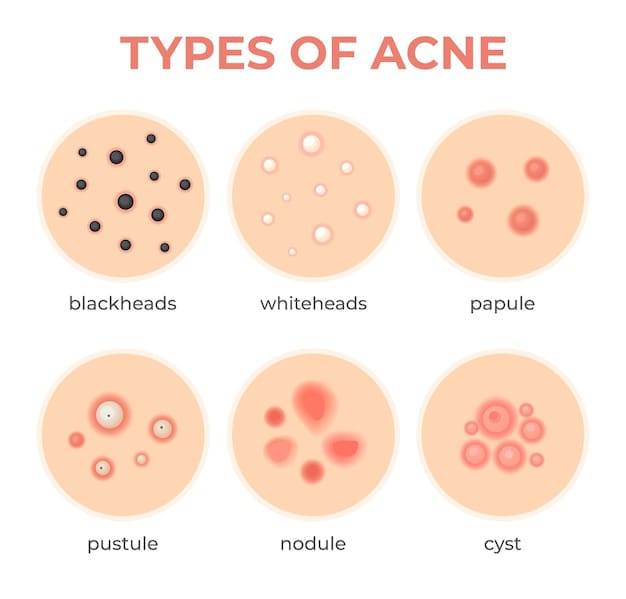
Acne vulgaris is one of the most common inflammatory skin troubles characterised by several skin lesions including clinicopathological changes such as comedones, papules, pustules , nodules, cystic lesions leading to ultimate result of scar formation.These lesions are usually appeared on face and may appear on back shoulders neck and chest.
Acne begins early in females, but is more severe in males. Acne usually persists until early 20’s, although in a few patients, it may even continue into the fifth decade. Acne is multifactorial in origin.
It is an inflammatory disorder of the pilosebaceous unit, which runs a chronic course and it is self-limiting. Acne vulgaris is triggered by Cutibacterium acnes in adolescence, under the influence of normal circulating dehydroepiandrosterone (DHEA). It is a very common skin disorder which can present with inflammatory and non-inflammatory lesions chiefly on the face but can also occur on the upper arms, trunk, and back.
ETIOLOGY
Acne occurs by hypersensitivity of the sebaceous glands to a normal circulating level of androgens, which are aggravated by P. acnes and inflammation. Causes of acne include the following:
- Use of medications like lithium, steroids, and anticonvulsants
- Exposure to excess sunlight
- Use of occlusive wear like shoulder pads, headbands backpacks, and underwire brassieres
- Endocrine disorders like polycystic ovarian syndrome and even pregnancy
- Genetic factors affect the percentage of branched fatty acids in sebum. Heritability estimates range from 50-90% .
- Environmental Factors It includes various factors like High-humidity, Prolonged sweating, Increase in skin hydration, Exposure to dirt or vaporized cooking oil or certain chemicals like petroleum derivatives.
- Psychological Studies shows that increased stress levels are associated with increased acne severity .
- Diet – The relationship between acne and diet remains unclear although high glycemic diet is associated with worsening of acne . There is a positive association between the milk consumption and prevalence of acne increases . Reports showed that consumption of chocolate and salt are not associated with development of acne .
EPIDEMIOLOGY
Acne may appear in adolescence, and it persists through the early thirties . Urban populations are more affected than rural populations. About 20% of the affected individuals develop severe acne, which results in scarring. Some races appear to be more affected than others. Asians and Africans tend to develop severe acne, but mild acne is more common in the white population. In general, populations with darker skin also tend to develop hyperpigmentation. Acne can also develop in neonates but in most cases, resolves spontaneously.
PATHOGENESIS
Acne develops as a result of bacterial overgrowth and inflammation in the pilosebaceous units. The body’s hormone level alter pilo sebaceous gland function and causes Acne Vulgaris . Follicular epithelial cells abnormally differentiated and forms tighter intracellular adhesions and shed less. That leads to the development of micro comedones or hyperkeratotic plugs which enlarge to form non inflammatory open or closed comedones . Androgens are causative factors for acne which induces sebum production leading to the comedones development . Changes in the skin’s natural flora are linked with androgen related sebum production. Diseases like congenital adrenal hyperplasia, polycystic ovarian syndrome and endocrine tumours result in a high level of androgens in body and associated with the development of acne vulgaris.
CLINICAL FEATURES
Acne occurs on centrofacial areas of the back, upper trunk, and deltoid region. Acne present as polymorphic lesions starting with comedones
Grade 1: Comedones. They are of two types, open and closed. Open comedones are due to plugging of the pilosebaceous orifice by sebum on the skin surface. Closed comedones are due to keratin and sebum plugging the pilosebaceous orifice below the skin surface.
Grade 2: Inflammatory lesions present as a small papule with erythema.
Grade 3: Pustules.
Grade 4: Many pustules coalesce to form nodules and cysts.
Acne can leave various scars after healing, which may present as depressed scars or hypertrophic and keloidal scars. Depressed scars may be gentle contour (boxcar scars) or ice pick scars, which are deep pits. Acne is associated with seborrhoea and in the case of hyperandrogenism associated with hirsutism, acanthosis nigricans, irregular menstrual period, and weight gain.
Acne vulgaris is diagnosed clinically. However, in women of childbearing age, one should ask for a history of hirsutism or dysmenorrhea. If positive, then levels of testosterone, LH, FSH, and DHEA should be ordered.
DIAGNOSIS AND EVALUATION
The diagnosis of AV is generally established by identifying of quantity and morphology of the lesions. Their morphologies are divided into the non inflammatory comedones , termed as open (blackheads) or closed (whiteheads) and the inflammatory lesions, termed as papules, pustules, cyst, or nodules. American Academy Dermatology (AAD) classified the severity of AV into mild, moderate, and severe.
DIFFERENTIAL DIAGNOSIS
There are several of differential diagnosis of
(1) Acne rosacea, which is commonly observed in middle age or later in life
(2) Folliculitis and boils, which often present with pustular lesions similar to acne
(3) Milia, which is a small non-follicular keratin papules that may be confused with whiteheads
(4) Pityrosporum folliculitis, which more predominates on the trunk.
MANAGEMENT
BERBERIS AQUIFOLIUM
Acne. Blotches and pimples. Clears the complexion.
KALIUM BROMATUM
Acne of face, pustules. Itching; worse on chest, shoulders, and face. Anæsthesia of skin.
PULSATILLA
Urticaria, after rich food , from delayed menses, worse undressing. Measles. Acne at puberty. Varicose veins.
CALCAREA CARB
Unhealthy; readily ulcerating; flaccid. Small wounds do not heal readily. Glands swollen. Nettle rash; better in cold air. Warts on face and hands. Petechial eruptions. Chilblains. Boils.
DULCAMARA
Pruritus, always worse in cold, wet weather. Herpes zoster, pemphigus. Swelling and indurated glands from cold. Vesicular eruptions. Sensitive bleeding ulcers. Little boils. Red spots, urticaria, brought on by exposure, or sour stomach. Humid eruptions on face, genitals, hands, etc. Warts, large, smooth, on face and palmar surface of hands. Anasarca. Thick, brown-yellow crusts, bleeding when scratched.
PSORINUM
Dirty, dingy look. Dry, lusterless, rough hair. Intolerable itching. Herpetic eruptions, especially on scalp and bends of joints with itching; worse, from warmth of bed. Enlarged glands. Sebaceous glands secrete excessively; oily skin. Indolent ulcers, slow to heal. Eczema behind ears. Crusty eruptions all over.
SULPHUR
Dry, scaly, unhealthy; every little injury suppurates. Freckles. Itching, burning; worse scratching and washing. Pimply eruption, pustules, hang-nails. Excoriation, especially in folds . Feeling of a band around bones. Skin affections after local medication. Pruritus, especially from warmth, is evening, often recurs in spring-time, in damp weather.
CONCLUSION This brief review highlights the relevant clinical findings and pathology of acne vulgaris as a chronic inflammatory skin disease affecting the pilosebaceous glands. It has multifactorial causes and manifestations varying from the mild to severe degree.
About Author
Dr. Adithya Asok NP, MD Scholar, Batch 2020-21, Department of Practice of Medicine, Government Homoeopathic Medical College and Hospital, Bhopal, Madhya Pradesh