ABSTRACT:
Loss of smell and taste are predominating symptoms of SARS Cov19 in more than half of the patients. This article reflects why and how COVID-19 cause these symptoms and why they are more profound in this disease. These symptoms are not merely loss of senses but act as deterrent for quality of life as a whole. It shows various coping strategies, rubrics and homoeopathic medicines which can prove beneficial or aid in healing these symptoms.
KEYWORDS: Loss of smell, loss of taste, SARS CoV, COVID 19, olfactory pathway, ACE receptors
ABBREVIATIONS: ACE- angiotensin converting enzyme, SARS CoV2- severe acute respiratory syndrome corona virus 2, TMPRSS2- Transmembrane serine protease 2, G Protein – guanine nucleotide- binding proteins, COVID-19 – coronavirus disease 2019, AMP – adenosine monophosphate.
INTRODUCTION:
All our five senses have major effect on us. Senses of smell and taste are in fact one composite sense. Sense of smell and taste are the oldest senses and close to the center of brain. Fresh air, fragrances of flowers, moist earth after rain, freshly baked cakes and cookies, and an endless list of other aromas can light up the brain’s pleasure centers or vice versa.
But COVID 19 infection has caused major loss of smell and taste. Total loss of smell and taste are known as anosmia and ageusia respectively. These symptoms of loss of smell and taste are very strange but hallmark symptoms, so much so that they are considered a better predictor of whether someone has been infected with COVID 19 or not than other common symptoms, such as fever, pain in throat or coughing. Studies suggest that up to half infected people temporarily lose their ability to perceive smells, although this might be as high as 67% in those with mild to moderate infections possibly because they are younger in age, and may be more sensitive to altered olfactory sense.
The recovery rate of these altered senses varies from few weeks to many months or even lifetime in rarest of cases. There is not much awareness of these symptoms in our society and this can lead to nutritional deficits and psychological effects. Recent treatments available for this such as steroidal medicines or sprays do not show any significant effect but it has been seen that some coping strategies are beneficial and in addition homoeopathic medicines can boost the healing [1]
DISCUSSION:
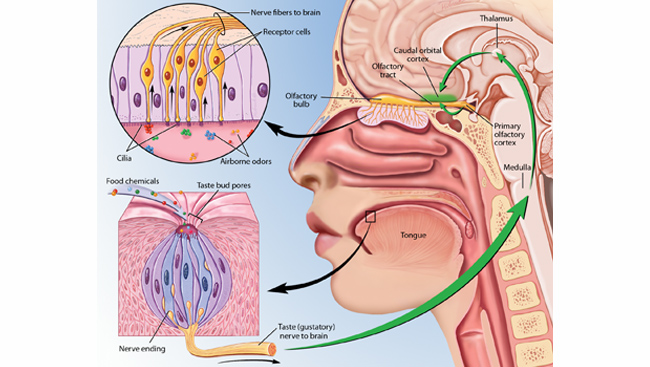
To understand, why there is loss of smell and taste in COVID infection, one has to first understand
the olfactory and taste pathway, how brain is able to perceive these senses.
OLFACTORY PATHWAY
[2]
- The way we sense odors is through a cluster of nerve cells called “olfactory sensory neurons/olfactory receptors”, which are situated in olfactory mucus membrane lining upper part of the nostrils. There are 10-20 million of olfactory receptor cells supported by sustentacular cells. The mucosa also contains mucus secreting Bowman’s glands.
- Olfactory receptor cell is a bipolar neuron with a short dendrite. These neurons have tiny hair-like projections cilia (10-12 cilia from each neuron) which extend out into the mucous-covered nasal lining and respond to odor molecules that we breathe out through our noses.
- Axons of bipolar olfactory receptors on each side of nose pierce the 20 olfactory foramina in cribriform plate of ethmoid bone.
- Then 40 or so bundles of axons form the right and left olfactory nerves.
- They terminate in brain in paired masses of gray matter called olfactory bulbs. (Below frontal lobe and lateral ethmoid bone). Here, they synapse with second order neurons to form olfactory tract.
- Then, these axons project to the lateral olfactory area (inferior and medial surface of temporal lobe) and most of them also ends here. This is also called primary olfactory area where conscious awareness of smell begins.
- Other axons terminate in olfactory cortex which includes both temporal lobe and parts of Limbic system.
- Connections to other limbic system regions and to hypothalamus account for emotional and memory evoked response to odours.
- Lateral olfactory area may extend to frontal lobe both directly and indirectly via thalamus.
- This area is called orbitofrontal area (area 11). It contains the secondary and tertiary olfactory cortical areas for odor identification and discrimination.
TASTE PATHWAY
- Receptors for taste sensation are on the taste buds
- First order neurons of taste pathway are in the nuclei of 3 different cranial nerves (facial nerve, glossopharyngeal nerve, vagus nerve)
- The impulses then propagate along these cranial nerves to the medulla oblangata
- From there, some axons carrying taste signals project to the limbic system and hypothalamus whereas others project to the thalamus
- Taste signals then project from the Thalamus to the primary gustatory area in parietal lobe of cerebral cortex. This area gives rise to conscious perception of taste.
- The primary taste cortex provides individual and combined representations of the taste, temperature, and texture (including viscosity and fat texture) of food within the mouth independently of hunger. One synapse on, in the orbitofrontal cortex, these sensory inputs are for some neurons combined by learning with olfactory and visual inputs
- In humans, the representation of food-related and other pleasant stimuli is found particularly in the medial orbitofrontal cortex. Different neurons respond to different combinations, providing an upscale representation of the sensory properties of food.
- Food intake is thus controlled by building a multimodal representation of the sensory properties of food in the orbitofrontal cortex, and gating this representation by satiety signals to produce a representation of the pleasantness or reward value of food which drives food intake. A neuronal representation of taste is also found in the pregenual cingulate cortex, which receives inputs from the orbitofrontal cortex. In humans many pleasant stimuli activate the pregenual cingulate cortex, pointing towards this as an important area in motivation and emotion. [3,4,5,6]
HOW OLFACTION AND TASTE SENSATIONS ARE INTER-RELATED?
- Taste and smell are separate senses with their individual receptor organs, yet they are intimately entwined.
- Olfactory and taste receptors are both chemoreceptors. They both perceive chemicals in air or in our food respectively. They both are stimulated by substances in dissolved state (in mucus or saliva).
- The nose and mouth are connected through the same airway which means that we taste and smell foods at the same time.
- Flavor perception is heavily influenced by our sense of smell, which is why holding nose can make unpalatable foods easier to swallow
- Olfactory and gustatory information when passes to and converge in adjacent parts of orbitofrontal cortex (common converging point) helps creating perception of different flavors
- The mechanism of generation of action potential in both pathways is almost same which is explained below:
OLFACTORY SENSATION:
- Airborne odor molecules called odorants are detected by olfactory receptor cell
- Molecules of dissolved odorants in mucus bind with receptor G-Proteins in the cilia
- They form substance receptor complex
- which activates adenyl cyclase
- Which in turn helps in formation of cyclic AMP
- It causes opening of Na channels leading to influx of Na+ and generation of receptor potential
- Which in turn generate Action potential in axon of bipolar neuron
- Humans have ability to recognize about 10,000 different odors probably depends on patterns of activity in the brain that arise from activation of many different combinations of olfactory receptors.
GUSTATORY SENSATION
Similarly, Tastants dissolved in saliva detected by taste buds
- Act on microvilli of taste receptors
- Then, they bind to receptors on plasma membrane that are linked to G-Proteins
- It then activates several different chemicals known as second messenger inside the gustatory receptor cell
- Different second messengers cause depolarization in several different ways which causes development of receptor potential
- This in turn, is responsible for generation of action potential
- Humans can detect 4 basic smells- Sweet, Salty, Bitter, Sour and Umami. Different tastes arise from the activation of different groups of taste neurons.
- In addition, although each individual gustatory receptor cell responds to more than one of the five prime tastes, it may respond more strongly to some tastants than to others. [3,4,5,6]
HOW COVID19 CAUSE LOSS OF SMELL AND TASTE?
In the initial days of Pandemic, scientists feared that SARS-CoV-2 might be triggering smell loss by infecting these olfactory neurons and then making its way into the brain, where it might cause lasting damage. But Further researches revealed that this is not exactly the case. Various studies are done and various ways by which virus is infected are studied:
- A team led by Sandeep Robert Datta, a neurobiologist at Harvard Medical School in Boston, Massachusetts, has zeroed in supporting cells called Sustentacular cells in nose that are probably what the virus is infecting. They encode genes for ACE2 receptor protein and proteases which act as gateway for virus to penetrate human cells. These both genes are present more in nasal cavity as compared to other organs or Bronchiolar cells and Lungs. They are present in olfactory neurons also but do not express in right pattern in them because of this the virus cannot bind to them.
- The gene ACE2 encodes ACE2- Angiotensin converting enzyme receptor protein which binds with virus surfaced anchored glycoprotein- spike S protein allowing fusion of virus with host membrane cells
- Another gene TMPRSS2 (Hoffmann) encodes for Protease (Furin) which helps in priming the spike protein of SARSCoV2 which enhance the virus ability to internalize into cells.
- But there might be other ways in which COVID-19 induces smell loss. For instance, a research team in Italy showed that smell and taste loss occur at the same time as an increase in blood levels of an inflammation-signaling molecule called Interleukin-6. And a post-mortem study published last December showed clear signs of inflammation, like leaky blood vessels, within olfactory bulbs of individuals who had Covid19 [7]
HOW SUPP0RTING CELLS ALTER SMELL PATHWAY
1)Sustentacular cells maintain the delicate balance of salt ions in the mucus which olfactory neurons need to send signals to the brain. When that balance is disrupted, it leads to shutdown of neuronal signaling.
2) Another function of supporting cells is to provide structural and metabolic support to the olfactory neurons. A recent study in hamsters suggested that when these support cells are invaded by SARS-CoV-2 it leads to massive infiltration of immune cells, followed by a disruption to the normal organization or structure of the nasal lining, including the loss of the hairlike projections cilia that the neurons use to detect odor molecules. [8]
PAROSMIA- ANOTHER SYMPTOM IN COVID 19
During recovery phase, mostly after 10-14 days, some people also report altered/ distorted/ unpleasant smell called as “parosmia” or olfactory distortion disorder. Many people who are recovering from COVID-19 report smelling a foul, fetid, rancid odor constantly without any source or even smelling an odorant that is not present called phantosmia. It’s a very disgusting and frustrating symptom of COVID 19 but it is usually a sign that your nerve cells are recovering.
When newly formed stem cells develop into neurons in the nose, they extend their axons, through tiny holes in the cribriform plate at the base of the skull and connect with a structure in the brain called the olfactory bulb. During that time, sometimes axons connect to the wrong place or miswiring occurs, causing erratic smell or parosmia. It is also believed to be occurred due to an impact of the infection on the olfactory nerves or area of brain which helps in interpreting odors and aromas,
So far, there’s not a huge amount of research on parosmia in COVID-19 patients. But an international study of people with recent smell loss, found that 7% of more than 4,000 respondents reported experiencing parosmia.
While most people recover their normal sense within two to four weeks, a considerable percentage (estimated at around 10%) develop long-term olfactory dysfunction which can last for several months and sadly it’s even permanent for some people. [9]
WHY LOSS OF SMELL AND TASTE IS MORE COMMON IN SARSCoV2 THAN OTHER SARS VIRUS DISEASES OR RESPIRATORY ILLNESSES?
Incidence of anosmia in COVID patients varies because of genetic factors, viral load, specificities and susceptibilities of different evaluating populations or methods used in analysis but it is more profound in SARS-CoV 2 than other viruses because:
SARS-CoV-2 has a significantly higher ACE2 binding affinity because of its 3-dimensional structure of its binding site which has a more compact conformation and improved binding stability, it has important cleavage site inserted at the boundary of the S1/S2 subunits of the spike S protein (a host proprotein convertase, furin). This polybasic furin-type cleavage site is unique which enhances the virus ability to internalize into cells. ACE2 of human population binds to the ectodomain of the SARS-CoV-2 spike glycoprotein with about 10- to 20-fold higher affinity than the S protein of the previous SARS-CoV [10]
HOW SYMPTOMS OF LOSS OF SMELL AND TASTE IN COVID 19 ARE DIFFERENT FROM OTHER ILLNESSES
1) Loss of smell and taste are more profound in COVID 19 infection as compared to Influenza or other viral respiratory illnesses. In loss of taste, patients cannot even distinguish between basic tastes such as bitter and sweet.
2) COVID 19 patients although lose their sense of smell and taste but they don’t have necessarily nasal congestion or running or blocked nose which are common in other respiratory illnesses and loss of smell is an associated symptom with these.
3) During other illnesses patients recover their symptoms as soon as nasal congestion subsides but in COVID 19 patients take longer time to regain their senses as damaged cells take time to regrow [11]
RECOVERY RATE
The nasal lining began to regrow or rebuild itself after 14 days so the good news is that patients can start recovering in this time but the sad part is it is still not clear how much exact time it will take to regrow completely. It varies also from one individual to individual. In some, it recovers in few days, in some it fluctuates for many months till it becomes normal completely, and in some it can take months to year also to recover. As these senses diminishes with age, they can take longer or not fully regained in elderly patients. Very rarest of all, it can cause permanent or lasting damage. So, one can say average span can be from 1 month to 1year or above. [1,11]
SIDE EFFECTS OF PERSISTING SYMPTOMS OF LOSS OF SMELL AND TASTE
“Mostly people do not acknowledge these senses until they lose it.”
- Patients will not be able to appreciate any flavours in the food.
- Unable to acknowledge any taste and smell in food, it leads to poor appetite and hence results in undesired weight loss, malnutrition or nutrient deficits.
- Losing two out of five senses affects quality of life.
- It can put patients at risk/danger also as they will not be able to detect spoiled food, dangerous chemicals, poisons, fire, etc.
- It can lead to psychological disorders also such as depression, social withdrawal, etc.
- It can lead to difficulty in making Intimacy with other people as there is inability to detect body odors and pheromones. [12]
COPING STRATEGIES [11]
Recovery of sense of smell and taste depend on how fast these sense receptors can regrow. So, following strategies mainly aim at accelerating this process of regrowth:
1) OLFACTORY TRAINING- repeated and deliberate sniffing of a set of odorants like lemon, coffee beans, eucalyptus, cloves, rose, cinnamon, other essential oils etc. for 20 sec each at least twice or thrice a day. While sniffing, try to recall its smell or experience with that particular odorant. Principle of mindfulness plays a very vital role here, focusing your thoughts on that odorant and evoking its sensation, will help to recover more quickly.
2) ZINC SUPPLEMENTS- zinc is necessary for catalytic activity of enzymes. protein synthesis and cell division. That’s why it can help in enhancing senses of smell and taste. [13]
3) OMEGA 3 POLYUNSATURATED FAT SUPPLEMENTATION can be helpful because of its neuroprotective effects which mediate through anti-oxidant and anti-inflammatory pathways. Example – sea food, nuts and seeds (flax seeds, chia seeds, mustard seeds, walnuts etc.), plant oils (canola oil, soybean oil etc.), eggs, cauliflower etc.
4) VITAMIN SUPPLEMENTS-Vitamin A and vitamin B12: both these vitamins have a decisive role in regeneration of olfactory receptor neurons and thus, they can help in improving smell and taste sensations.
Vitamin D supplements: It helps in immunomodulation, improving lung function and is anti-viral in nature. It acts as a neurosteroid hormone that binds to vitamin D receptors in brain, spinal cord and olfactory network
Various studies also confirmed that Vitamin D supplementation helps in improving anosmia [14]
5) GINKGO BILOBA- It improves senses of smell and taste as it acts as an anti-oxidant, improves blood circulation and its sphere of action incudes nervous system and memory areas.
6) SODIUM CITRATE- Sodium citrate reduces free intranasal calcium and is, therefore, thought to prevent calcium-mediated feedback inhibition at the level of the olfactory receptor
7) ALPHA LIPOIC ACID- It is said to be universal anti-oxidant and thus helps in improving smell and taste sensations.
8) DIFFERENT YOGA ASANAS AND BREATHING EXERCISES like “anulom vilom” can prove beneficial in improving these senses.
9) Experiment with variety of foods, different colors, textures, aromatic herbs and spices, foods having strong flavors or smell.
10) Patients should Accept and acknowledge the feelings for the loss of senses and inculcate the feeling of gratitude that no other severe fatal symptoms or complication have occurred.
11) Maintain HOPEFULNESS AND PATIENCE for the recovery as it can take longer time than expected
HOMOEOPATHIC MANAGEMENT
Homoeopathy has specific remedies for these symptoms which can help in promoting healing. Various rubrics covering these symptoms are discussed below from different repertories:
Murphy3, Nose; SMELL, general; loss, of smell, wanting (110) ail, alum, alum-p, alum-sil, am-m, amyg-p, anac, ant-c, ant-s, ant-t, apoc-a, arg-n, arist-cl, arn, ars, ars-i, ars-s-f, arund, aspar, aur, aur-ar, aur-i, aur-s, BELL, bry, bufo, CALC, calc-i, CALC-S, calc-sil, camph, caps, carb-an, carbn-s, card-m, caust, cham, chel, chlor, cina, cocc, cod, con, cupr, cycl, elaps, graph, hell, HEP, hyos, ign, iod, ip, joan, just, kali-bi, kali-c, kali-i, kali-n, kali-p, kali-s, kali-sil, lach, laur, lem-m, lyc, mag-m, mag-p, mang, med, MERC, mez, morg, nat-ar, nat-c, NAT-M, nit-ac, nux-m, nux-v, olnd, op, phel, PHOS, PLB, psor, PULS, rhod, rhus-t, ruta, sabad, sang, sarr, sec, sel, SEP, SIL, spig, squil, staph, stict, stram, sul-ac, sul-i, sulph, syc-co, tarent-c, teucr, verat, ZINC, zinc-m,
Murphy3, Nose; SMELL, general; loss, of smell, wanting; catarrh, from (12) alum, calc, hep, just, mez, nat-m, nux-v, puls, sang, sep, sil, sulph,
Murphy3, Nose; SMELL, general; loss, of smell, wanting; taste, with loss of (8) amyg-p, ant-t, hyos, just, mag-m, nat-m, puls, rhod,
Murphy3, Taste; LOSS of taste; BELL, PHOS, NAT-M, PULS, SIL, ZINC, anac, ant-c, ant-t, apis, aur, bor, bry, calc, canth, crot-h, cycl, hep, hyos, kali-bi, mag-m, merc, nux-m, nux-v, par, pers, psor, sep, sul-ac, sulph, verat.
Murphy3, SMELL, Gen, odors, imaginary and real, bad, within nose; aur, bell, calc, canth, con, kali-bi, nit-ac, nux-v, phos, plb, puls, sulph
Combined, Mouth; TASTE; wanting; loss of taste (66) aeth, all-c, alum, am-m, anac, ant-c, ant-t, apis, ars, aur, aur-m, BELL, bor, bry, cact, calc, calc-ar, cann-s, canth, chin, cocc, coff, crot-h, cupr, cycl, dros, hep, hyos, ip, kali-bi, kali-br, kali-s, kreos, lyc, mag-c, mag-m, merc, merl, NAT-M, nat-s, nux-m, nux-v, op, ox-ac, par, PHOS, plan, podo, posit, psor, ptel, PULS, rheum, rhod, sabad, sang, sec, sep, SIL, stram, sul-ac, sulph, syph, ther, thuj, verat,
Boenninghausen; NOSE, SMELL, WEAK WITH, LOSS OF TASTE (7) PULS, ant-t, nat-m, hyos, just, mag-m, rhod.
Boenninghausen; NOSE, CORYZA, CONCOMITANTS, TASTE LOSS OF (7) NAT-M, PULS, am-m, ant-t, mag-m, rhod, sabad
Boericke, Nose; SENSE, OF SMELL, PAROSMIA (ILLUSIONS) (20) agn, ANAC, apoc-a, ars, aur, BELL, calc, cor-r, dios, graph, ign, KALI-BI, mag-m, MERC, nit-ac, nux-v, PHOS, PULS, sang, sulph,
[15]CONCLUSION
Thus, we conclude that it is the supporting/sustentacular cells which are damaged in COVID 19 which in turn disrupt transmission of nerve impulses along olfactory neurons and ultimately loss of smell occurs. As olfactory and gustatory pathways are inter connected and synapse in the end on orbitofrontal area, both the senses are affected simultaneously. These symptoms are more profound in COVID 19 as SARS CoV 2 has more affinity towards ACE2 receptors on supporting cells of nasal mucus membranes.
These symptoms are not merely loss of sensations only but they can affect quality of life including mental/emotional level also. In present scenario, allopathic sphere only provides oral steroids or steroidal nasal sprays which does not show any reliable results as per recent evidence-based studies. But various other strategies, nutrient supplements and smell training prove a beneficial role. Along with this, one can add homoeopathic medicines which can aid in healing process. The most common homoeopathic medicines suited for it are Pulsatilla nigricans, Natrum-muriaticum, Zincum-metallicum, Nux-vomica, Phosphorus, etc.
Better understanding of this will result in increasing awareness and encourage more coping strategies and better treatment options esp. homoeopathic medicines
REFERENCES:
- Geddes L. why covid 19 makes you lose your sense of smell and how to get it back. Gavi, the vaccine alliance; 2021, 23 Mar
Available from, URL: https://www.gavi.org/vaccineswork/why-covid-19-makes-you-lose-your-sense-smell-and-how-get-it-back
- Kibiuk.L.V, Stuart D.Brainfacts.org.[image on the internet].2012,1 Apr
Available from, URL:https://www.brainfacts.org/thinking-sensing-and-behaving/taste
- Tortora GJ, Grabowski SR. Principles of Anatomy and Physiology. Tenth Edition. U.S.A. John Wiley and Sons, Inc. 2003
- Sembulingam K, Sembulingum Prema. Essentials Of Medical Physiology. Third Edition. Jaypee Publications. 2003
- Rolls ET. Functions of the orbitofrontal and pregenual cingulate cortex in taste, olfaction, appetite and emotion. Acta Physiol Hung. 2008 Jun;95(2):131-64. doi: 10.1556/APhysiol.95.2008.2.1. PMID: 18642756
Available from, URL: https://pubmed.ncbi.nlm.nih.gov/18642756/
- Rolls ET. The functions of the orbitofrontal cortex. Brain Cogn. 2004 Jun;55(1):11-29. doi: 10.1016/S0278-2626(03)00277-X. PMID: 15134840.
Available from, URL: https://pubmed.ncbi.nlm.nih.gov/15134840/
- Jiang K. How Covid19 causes loss of smell. Harvard Medical School; 2020,24 july
Available from, URL: https://hms.harvard.edu/news/how-covid-19-causes-loss-smell
- Butowt R, von Bartheld CS. Anosmia in COVID-19: Underlying Mechanisms and Assessment of an Olfactory Route to Brain Infection. Neuroscientist. 2020 Sep 11:1073858420956905. doi: 10.1177/1073858420956905. Epub ahead of print. PMID: 32914699; PMCID: PMC7488171.
Available from; URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7488171/
9. Nazario B. What is parosmia?. WebMD;2021,24 Mar
Available from, URL:https://www.webmd.com/brain/
what-is-parosmia
10.Medina-Enriquez,M.M.,Lopez-Leon,S.,Carlos-Escalante, J.A.et al. ACE2: the
molecular doorway to SARS-CoV2. Cell.Biosci 10,148 (2020).
Available from, URL; https://doi.org/10-1186/313578-020-00519-
11. Newhouse L. Coping with the loss of smell and taste. Harvard Health Blog. 2020, 19
Oct
Available from, URL: https://www.health.harvard.edu/blog/coping-with-the-loss- of- sense-of- smell-and-taste-2020101921141
12. Mcdermott A.This is what its like to live without your sense of smell. Healthline;
2018, 2 Nov Available from, URL: https://www.healthline.com/health/anosmia
13. National Institute of Health. Office of Dietary Supplements. Zinc. 2021, 26 Mar
Available from; URL:https://ods.od.nih.gov/factsheets/ZincHealth%20Professional/
14. Kruse, Ralph A, and Jerrilyn A Cambron. “A possible correlation between vitamin D
deficiency and loss of smell: 2 case reports.” Journal of chiropractic medicine vol.
10,4 (2011): 310-5. doi:10.1016/j.jcm.2011.06.006
Available from, URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3315864/
15. David witko. Vision repertory software (Miccant) Patent: Dr Pravin Jain, 2005
About Author:
Dr Aditi Goyal, M.D(Hom)
Associate Professor, Repertory Department
Bakson Homoeopathic Medical Collge, Greater Noida





