Authors: Dr Pramod Singh1 Dr Poonam Sharma2 Dr Dushyant Kumar 3 Dr Abhishek 4 Dr Geeta Sharma5
ABSTRACT:
Migraine is a common brain disorder with high disability rates which involves a series of abnormal neuronal networks, interacting at different levels of the central and peripheral nervous system. An increase in the interest around migraine pathophysiology has allowed researchers to unravel certain neurophysiological mechanisms and neurotransmitter involvement culminating in the recent development of novel therapies, which might substantially change the clinical approach to migraine patients. Two types of migraines are seen generally classical migraine – a migraine with an aura or warning and common migraine – a migraine without an aura. The pharmacological treatment of migraine may be acute or preventive. Frequent severe and long lasting migraine attacks require prophylaxis. The better knowledge about migraine pathophysiology led us to discuss new treatment options. Migraine can be diagnosed by the symptoms like intense headache, relentless, throbbing pain, inability to carry out daily activities etc. Migraine attacks are treated with nonsteroidal anti-inflammatory drugs (NSAIDS), or triptans. Non-pharmacological treatment includes cognitive behavioural therapy, Complementary Treatments, yoga therapy etc.
KEYWORDS: Migraine, Pathophysiology, Pharmacological & Homeopathic Managemen
INTRODUCTION:
Ancient references to headache, migraine, and neuralgia can be found in the Ebers Papyrus (1200 B.C.), and evidence of trepanation of 9000 year old Neolithic skulls suggests the first headache treatment. Visual symptoms associated with headache were described by Hippocrates in 400 B.C., and Aretaeus provided one of the earliest classifications of headache around 200 AD. Migraine is the most common neurological cause of disability in the world. Migraine is a pervasive and debilitating, chronic neurological painful disorder, affecting from 15% to 29% of the general population.1,2 (10% of adult population in United States) Migraine is the second most common cause of headache characterized by recurrent episodes of headache and associated symptoms i.e., nausea, sensitivity to light and noise that typically last from 4 to 72 hours. Pain management of migraine includes both non-pharmacological and pharmacologic methods for acute episodes and prophylaxis. Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage. Pain is a dynamic complex process which is generally classified in terms of nociceptive and neuropathic pathways, migraine pain is a neuropathic pathways which is quiet different from nociceptive pain which is sustained by abnormal processing of sensory input by peripheral or CNS, a large number neuropathic pain syndromes exist and clinically ,they are often difficult to treat patients presents with spontaneous pain transmissions often described as tingling, burning, shockline or shooting, exaggerated painful response to normally non-noxious stimuli (Allodynia) or painful repoint to noxious stimuli (hyperalgesia). It is a common, chronic, incapacitating neurovascular disorder, characterized by attacks of severe headache, autonomic nervous system dysfunction, and in some patients, an aura involving neurologic symptoms.3,4 Recent advances in basic and applied clinical neuroscience have led to the development of a new class of selective serotonin (5-hydroxytryptamine [5-HT]) receptor agonists that activate 5-HT1B and 5-HT1D (5-HT1B/1D) receptors and are known as the triptans; these agents have changed the lives of countless patients with migraine. Despite such progress, migraine remains under diagnosed and the available therapies underuse.5,6
Epidemiology
Headache is a painful and common symptom. A number of primary headache disorders have been characterized, including tension-type headache, migraine and cluster headache, and overall these disorders account for approximately 95% of all headache complaints.7 Worldwide, migraines affect nearly 15% or approximately one billion people. It is more common in women at 19% than men at 11%. In the United States, about 6% of men and 18% of women get a migraine in a given year, with a lifetime risk of about 18% and 43% respectively. In Europe, migraines affect 12–28% of people at some point in their lives with about 6–15% of adult men and 14–35% of adult women getting at least one yearly. Rates of migraines are slightly lower in Asia and Africa than in Western countries.8 Chronic migraines occur in approximately 1.4 to 2.2% of the population. There is scarcity of Indian data on the epidemiology of migraine. The prevalence of migraine is 17.6% in females and 6% in males in the US. In an urban headache clinic 47% of the patients were found to have migraine without aura and 4% migraine with aura. Indian data for the incidence of migraine with aura seem to be lower when compared with data from other parts or the world.9
PATHOPHYSIOLOGY:
Migraine is best understood as a primary disorder of the brain. It is a form of neurovascular headache: a disorder in which neural events result in the dilation of blood vessels, which, in turn, results in pain and further nerve activation. Migraine is not caused by a primary vascular event. Migraine attacks are episodic and vary within and among patients. We may best explain this variability by considering the basic biologic problem in migraine to be the dysfunction of an ion channel in the aminergic brain-stem nuclei that normally modulates sensory input and exerts neural influences on cranial vessels. In patients with familial hemiplegic migraine, missense mutations in the subunit of the voltage-gated P/Q-type calcium channel have been identified. It is possible that other ion-channel mutations contribute to migraine without aura, since it is primarily cases of migraine with aura that have been linked to the familial-hemiplegic-migraine locus. It thus seems possible that the aura of migraine is separate from the headache, with aura susceptibility genes as its determinant; the pain and associated features of migraine itself may be determined by another gene or genes.
Migraine and the Brain
As noted above, migraine probably results from a dysfunction of brain-stem or diencephalic nuclei that are involved in the sensory — particularly nociceptive — modulation of craniovascular afferents. Activation in the brain stem during attacks of migraine has been detected with the use of positron-emission tomography. Moreover, the aura of migraine is likely to be the human counterpart of the animal phenomenon of Leão’s spreading depression. Aura is characterized by a wave of oligemia that passes across the cortex at the characteristically slow rate of 2 to 6 mm per minute. A short phase of hyperemia precedes this oligemia and is likely to be a correlate of such symptoms as flashing, jagged lights. Oligemia is a response to depressed neuronal function and is still clearly present when the headache starts. These findings, together with direct evidence that the local oxygen supply is more than adequate, make the notion that migraine is simply a vascular headache untenable10 (Fig. 1).
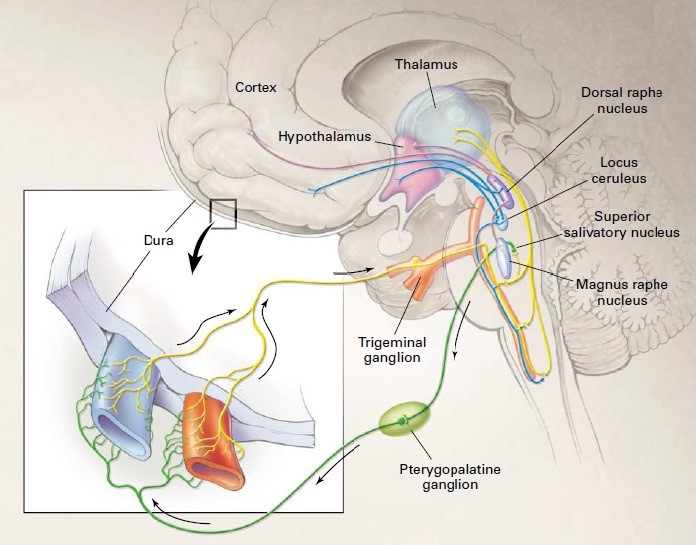
Figure 1: Migraine involves dysfunction of brain-stem pathways that normally modulate sensory input. The key pathways for the pain are the trigeminovascular input from the meningeal vessels, which passes through the trigeminal ganglion and synapses on secondorder neurons in the trigeminocervical complex. These neurons, in turn, project through the quintothalamic tract, and after decussating in the brain stem, form synapses with neurons in the thalamus. There is a reflex connection between neurons in the pons in the superior salivatory nucleus, which results in a cranial parasympathetic outflow that is mediated through the pterygopalatine, otic, and carotid ganglia. This trigeminal–autonomic reflex is present in normal persons and is expressed most strongly in patients with trigeminal–autonomic cephalgias, such as cluster headache and paroxysmal hemicrania; it may be active in migraine. Brain imaging studies suggest that important modulation of the trigeminovascular nociceptive input comes from the dorsal raphe nucleus, locus ceruleus, and nucleus raphe magnus.
TYPES OF MIGRAINE:
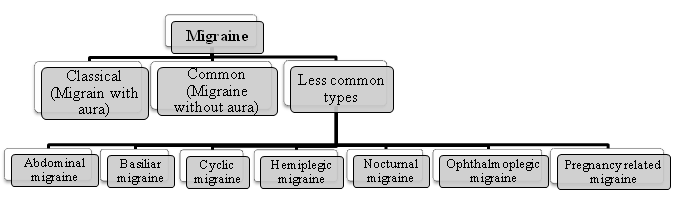
Classical migraine:
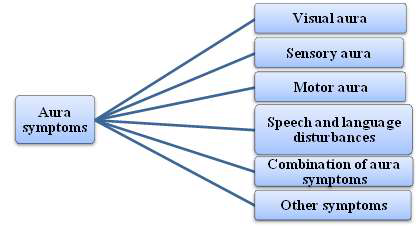
Classical migraine (migraine with aura) less number of migraine patients (20%) experiences the aura, which is the term of sign of occurrence of the pain. These can be described as the spots or the zigzag lines before the eyes associated with blurred vision. These symptoms go away usually within one hour and are replaced by a headache. One or more fully reversible aura symptoms indicating brain dysfunction. At least one aura symptom develops gradually over more than 4 minutes or 2 or more symptoms occur in succession. No single aura symptom lasts more than 60 minutes. Headache follows aura with a free interval of less than 60 minutes (it may also begin before or with the aura). Most migraineurs with aura also have migraine without aura. Total duration of the aura is usually less than 1 hour. If the aura lasts more than 1 hour but less than 1 week, then it is „„migraine with prolonged aura‟‟ (also termed „„complicated migraine‟‟).
Common migraine:
Headaches begin without warnings in common migraine. This was mostly seen in children. Headache has at least two of the following characteristics:
- Unilateral location
- Pulsating quality
- Moderate or severe intensity (inhibits or prohibits daily activities)
- Aggravation by walking stairs or similar routine physical activity
Less common types:
1. Abdominal migraine
- Also known as periodic syndrome
- Abdominal pain lasting for 1-72 hours along with nausea, vomiting, flushing or pallor.
2. Basiliar migraine
- Pain arises from brain stem.
- Symptoms like dizziness, double vision, tingling on both sides of body are seen in this type.
3. Cyclic migraine
- Long lasting attacks (10 or more /month)
- Careful monitoring of blood level and thyroid functioning is needed.
4. Hemiplegic migraine
- Severe type of migraine causes temporary motor paralysis.
- Sensory disturbances on one side of the body followed by headache.
5. Nocturnal migraine
- Attacks during early in the morning or middle in the night often awaken patients from sleep.
6. Ophthalmoplegic migraine
- The pain usually surrounds eyeball and lasts from a few days to few months.
- It is caused by the weakness of the muscles surrounding the eye.
7. Pregnancy related migraine
- Migraine attacks from the 3rd month of pregnancy till delivery due to hormonal stability.
- Non medical treatment was effective in this case.11
EXAMINATION AND INVESTIGATIONS:
The main goal of examination and investigation is to consider brain disease and to screen out hypertension and depression along with exclusion of causes of migraine like symptoms but no tests to confirm migraine.12,13 Investigations include brain scan which is referral to find the early diagnosing of neurological disorders which provides impossible workload of 18% women, 6% men have migraine, 3% have chronic daily headache. Other tests include erythrocyte sedimentation rate (ESR) in early headache of geriatrics which address temporal arteritis and chest X-ray in smokers to consider metastatic cancer.14,15
TREATMENT:
- PHARMACOLOGICAL TREATMENT:
1. Pain relievers – Ibuprofen, Acetaminophen Combination of acetaminophen, aspirin and caffeine may ease moderate pain but are not effective for severe migraines. If taken for long periods, these can lead to ulcers, gastro intestinal bleeding and rebound headaches.
2. Triptans – Sumatriptan, Rizotriptan, Almotriptan, Zolmitriptan, Frovatriptan and eletriptan. Combination of sumatriptan and naproxen sodium (treximet) has proved effective in relieving migraine symptoms than individual medications.
3. Ergot – Combination of ergotamine and caffeine (migrergot, cafergot) are less expensive and also less effective than Triptans. They are most effective where pain lasts for more than 48hrs. Dihydroergotamine is more effective and has fewer side effects than ergotamine. It is also available as nasal spray and in injection form.
4. Anti-Nausea – Medication for nausea is appropriate and usually combined with other drugs. Metoclopromide or prochlorperazine are frequently prescribed medications.
5. Opiates – Narcotics, particularly codeine are sometimes used to treat migraine headache pain when people can‟t take ergots or Triptans.
6. Butalbital Combinations – Medications that combine the sedative Butalbital with aspirin/acetaminophen are sometimes used to treat migraine attacks. Some combinations also include caffeine or codeine.
7. Cardiovascular drugs – Anti-hypertensive medications like lisinopril, candesartan are useful in decreasing the frequency and severity of migraines. - blockers and calcium channel blockers like verapamil are also used.
8. Anti-depressants – Tricyclic antidepressants like amitriptyline, nortriptyline and protriptyline are most effective in preventing certain headaches including migraines. They act by affecting the level of serotonin and other brain chemicals.
9. Anti-seizure drugs – Divalproex and topirmate and gaba-pentene reduce the frequency of migraines.
10. Cyproheptadine – These anti histamines specifically affect the serotonin activity. Physicians sometimes give it to children as a preventive measure.
11. Botulinum Toxin – It is used as treatment for chronic migraines. Injections are made in the muscles of forehead and the neck. When this is shown to be effective, the treatment typically needs to be repeated every 3 months.16
- HOMEOPATHIC MANAGEMENT:
Spigelia Anthelmia
Spigelia mainly left sided remedy. Pain beneath frontal eminence and temples extending to eyes. Semi-lateral involvement. Pain is violent, throbbing type. Pain as if band around head. Hearing exalted. Pain worse from motion, touch.
Lachesis
Left sided migraines. Headache are often worst before the menstrual period and better once the flow begins. Pain through head on awaking. Feel pressure and burning on vertex Face is very pale. Pain worse after sleep.
Cyclamen
Migraines that start with flickering in the eyes. Pain in often right sided and involve in the ear. Frequent sneezing with itching in ear.. Dim vision or dizziness. Person is very sympathetic and emotional. Depression with weeping desire to be alone.
Coffea Cruda
Bad effects of sudden emotions surprises, joy. Pain worse from noise, smell. Seems as if brain were torn to pieces as iif nail were driven in head. Patient is over sensitive.
Cimicifuga
Migraines with throbbing pain (as if the top of the head would fly open). Shooting pain in the eyes. Headache are often associated with the menstrual period. Migraine due to over study or worrying. Ears sensitive to least noise.
Sepia Officinalis
Left sided migraine. Dizziness and nausea. Worse from missing meals and worse near menstrual period. Congestive type of headache. Feels better on lying down. Headache is worse from stooping, motion coughing, going up stairs. Pain better from tight bandage. Headache relieved from vomiting.
Sanguinaria
Right sided migraine. Pain worse from sun exposure. Pain extending to the forehead with a bursting feeling in the eye. Worse from noise, light. Headache improve after vomiting. Headache return at climacteric. Pain with burning in eyes.
Natrum Muriaticum
Migraines right sided. Worse from grief or emotional upsets. Worse from sunrise to sunset. Anaemic headache. Congestive type of pain. Headache feels like a thousand little hammers were knocking on the brain. Numb and tingling feeling before headache starts. Pain is better lying in the dark.
Iris Versicolor
Intense migraines with blurry vision. Headache with vomiting. Sick type of headache and induce by eating anything. Sensation of constriction around the forehead. Worse from rest.
Ignatia
Headache after emotional upsets or caused by grief. Congestive type of headache. Worse from smoking, smelling tobacco. Cramp-like pain over root of nose. Headache is often focused on one side of the head, may feel as if a nail is driven.
Glonoinum
Headache with confusion and dizziness. Throbbing type of pain. Effects of sunstroke. Head feels heavy but cannot lay it on pillow. Cannot bear any heat. Feels better from uncovering head. Pain is increasing and decreasing with the sun. Headache in place of menses.
Belladonna
Headache worse on right side. Throbbing type of pain. Vertigo with falling to left side or backwards. Pain worse from light, noise, jar, lying down and better by pressure. Sudden and violent attack of headache. Headache from suppressed catarrhal flow. Pain fullness especially in forehead and also occiput and temples.
Gelsemium
Congestive type of headache. Dull heavy ache with heaviness of eyelids. Pain in temple extending into ears and wing of nose. Headache preceded by blindness and better, profuse urination. Headache with dizziness, drowsiness, muscular weakness. Pain is better by compression and lying with head high.17
- ALTERNATIVE THERAPY:
Cognitive Behavioral Therapy (CBT):
It is based on principle that anxiety and distress are aggravators of an evolving migraine headache. It is designed to help patient identify and modify maladaptive response that may trigger or aggravate a migraine headache.18
Complementary Treatments:
These include acupuncture or acupressure, massage, exercise and chiropractic, herbs etc.
Yoga therapy:
Yoga, coupling physical exercise and breathing, meditation are the alternative form of mind body therapy and used to lower the symptoms of chronic pain, emotional stress, anxiety and depression.
Lifestyle Modifications:
Lifestyle impacts the severity and frequency of migraine can be understanding and useful for successful prevention of migraine.19
Sleep:
Maintain consistent sleep patterns, including weekend and holidays.
Exercise:
A routine of 20-40 minutes of aerobic exercise can relieve stress and maintain balance internal physiology.
Eating:
Have and maintain meals regularly and properly with good diet.
Reduce stress and increase posture:
Reduce stress with yoga, meditation and maintain posture that imparts migraine triggers.20
CONCLUSION:
The recent recognition of migraine as a debilitating neurological condition is an important advance in directing more resources to the development of new treatments and their deployment to patients. The last two decades have seen a number of important studies in the area of primary headaches leading to an extremely exciting era for researchers interested in this disorder. The pharmacological treatment of migraine can be acute (abortive) or preventive, and patients with frequent severe headaches often require both approaches. Acute migraine attacks are treated with non-steroidal anti-inflammatory drugs (NSAIDS), or triptans. Adjunctive antiemetic therapy is useful for combating the nausea and vomiting that accompany migraine headache. Preventive treatment is used to reduce the frequency, duration or severity of attacks includes beta blockers, serotonin antagonist, antidepressant, antiepileptic, and non-pharmacological therapy. New treatments are rapidly becoming available for patients and a better understanding of its pathophysiological mechanisms is allowing a greater awareness of the complexity of a brain disease which has often been overlooked and undermanaged.
REFERENCE:
- Campillo D. Neurosurgical pathology in prehistory. Acta Neurochir (Wien). 1984; 70:275-290.
- Magiorkinis E, Diamantis A, Mitsikostas DD, Androutsos G. Headaches in antiquity and during early scientific era. J Neurol. 2009; 256:1215- 1220.
- Global Burden of Disease Study 2013 Collaborators (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (Lond, Engl) 386:743–800
- Goadsby PJ. Bench to bedside advances in the 21st century for primary headache disorders: migraine treatments for\ migraine patients. Brain. 2006; 139:2571–2577.
- Lance JW, Goadsby PJ. Mechanism and management of headache. 6th ed. Boston: Butterworth–Heinemann, 1998.
- Silberstein SD, Lipton RB, Goadsby PJ. Headache in clinical practice. Oxford, England: Isis Medical Media, 1998.
- Mateen FJ, Dua T, Steiner T, Saxena S; Headache disorders in developing countries: research over the past decade. Cephalalgia, 2008;28(11):1107-1114
- Stovner LJ, Zwart JA, Hagen K, Terwindt GM, Pascual J; Epidemiology of headache in Europe. European Journal of Neurology,2006;13(4):333- 345.
- Ravishankar K; Recent trends in migraine management. Insignal RK ed.update medicine. The association of physicians of India.Vol 17:New Delhi; Jaypee Brothers.
- Alastair J., WOOD J. Migraine Current Understanding and Management. Drug Therapy. N Engl J Med, 2002; 346 (4) 257-270.
- Wessman M, Terwindt GM, Kaunisto MA, Palotie A, Ophoff RA; Migraine-A complex review. Migraine: a complex genetic disorder. Lancet Neurol, 2007;6(6):521-532.
- Jeffree RL, Besser M. Colloid cyst of the third ventricle: a clinical review of 39 cases. J Clin Neurosci 2001;8:328–31.
- Stoodley MA, Nguyen TP, Robbins P. Familial fatal and near-fatal third ventricle colloid cysts. Aust NZ J Surg 1999;10:733–6.
- Pollock BE, Huston J 3rd. Natural history of asymptomatic colloid cysts of the third ventricle. J Neurosurg 1999;91:364–9.
- .E Khoury C, Brugieres P, Decq P. Colloid cysts of the third ventricle: are MR imaging patterns predictive of difficulty with percutaneous treatment. J Neuroradiol 2000;21:489–92.
- B. Prameela, S. Subhashini, V. Anusha, D. Eswar Tony, N. Rama Rao, Migraine – A Malady: A Short Review. Sch. Acad. J. Pharm., 2014; 3(3): 285-289.
- Boericke W. New manual of homeopathic materia medica with repertory. New Delhi B. Jain Publishers Pvt . Ltd. 2000.
- Muthyala N., et al. “Migraine and Migraine Management: A Review”. Pharma Tutor 6 2018: 8-17.
- Stewart J., et al. “Mechanisms of Action of the 5-HT1B/1D Receptor Agonists”. Archives of Neurology 59 (2002): 1084-1088.
- Selby G and Lance JW. “Observations on 500 cases of migraine vand allied vascular headache”. Journal of Neurology Neurosurgery Psychiatry 23 (1960): 23-32.
Authors: Dr Pramod Singh1 Dr Poonam Sharma2 Dr Dushyant Kumar 3 Dr Abhishek 4 Dr Geeta Sharma5
1.Head of Department , Department of Homoeopathic pharmacy , Dr.M.P.K Homoeopathic Medical college Hospital and research centre Saipura ,Jaipur
2.MD scholar , Department of Homoeopathic pharmacy , Dr.M.P.K Homoeopathic Medical college Hospital and research centre Saipura ,Jaipur
3MD scholar , Department of Homoeopathic pharmacy , Dr.M.P.K Homoeopathic Medical college Hospital and research centre Saipura ,Jaipur
4 MD scholar , Department of Homoeopathic pharmacy , Dr.M.P.K Homoeopathic Medical college Hospital and research centre Saipura , Jaipur
5.MD scholar , Department of Homoeopathic pharmacy , Dr.M.P.K Homoeopathic Medical college Hospital and research centre Saipura , Jaipur