Essentials of Community Medicine: Fixing our inverted public health pyramid.
METHODS AND MATERIALS
- Times of India News Paper
- OPD Pandit Jawahar Lal Nehru Homeopathic Medical College and Hospital, Kanpur.
- Community Health Survey and Visits.
- “Ayush Apke Dwar” health checkup camps.
- School health and family visits.
AIMS AND OBJECTIVES
- To evaluate the access, service delivery and qualitative strong foundation of health and wellness centers (HWC) i.e. “First point of contact centers”.
- To specify innovative interventions and concerted efforts towards :-
- Plugging the rural – urban inequality.
- Skewed doctor – patient ratio.
- To design a prophylaxis in order to improve India’s health care system by rationally collaborating the PPP model (Public Private Partnership Model)
“The catch in our breath when we are startled, the tension in our guts when we are worried, the exhaustion we feel from our anxiety, are all as much a part of our illnesses as are the bacteria & viruses which attack us and can, in fact be just as debilitating, just as deadly.”
“SEENE MEIN JALAN, DIL MEIN TUFAN SA KYUN HAI
IS SHAHAR MEIN, HAR SHAKS PARESHAN SA KYUN HAI ?”
Life is full of ironies, esp. in the realm of health. It is often difficult to predict which person will become sick & which one will remain healthy. Life can be stressful. Everyone faces a different mix of demands & adjustments in life & any of us may breakdown if the going gets tough enough.
“TODAY’S STRESS CAN BE TOMORROW’S VULNERABILITY”
People are not disturbed by situations per se, but by the ways they appraise and react to situations. In stress, a demand exceeds a person’s coping abilities, resulting in reactions such as disturbances of cognition, emotion & behavior that can adversely affect well-being. Trauma freezes people in time. Years after trauma is over, people are still living it.
Every day we see seeds sprouting, flowers blooming, fruits ripening but we do not want to think about how it happens. There is a power that does this work; it’s the all-pervading power of divine love. Now, the time has come to feel this power through the instrument within us. This instrument has no use unless it is connected to the supreme divine power. We don’t know our potential, our beauty; however, once the connection with the supreme power is established, we will be surprised at the dynamic results. Human awareness can be developed to a higher dimension through this art of healing and it is becoming, evolving……..
Community medicine is the beating heart of the medical fraternity. New millennium has given wealth of study matter yet it is best taught practically in community than theory.
Medicine is in a state of flux and the physicians to a great extent are prisoners of the drug manufacturers; the time is ripe for a change in the quality of medical services now being furnished to the citizens of our country. So I plead to you in plain words – get off your stern & begin to make the substantial change!
The last few decades have been an extraordinary period of change and growth in terms of clinical provision of medical care in India. We see here some of the very best tertiary care in the world, to some extent even primary care. On the research side, however, India has a very long way to go. That’s partial because there hasn’t been a strong tradition & culture of research here. Funding, support & training of young researchers are lacking. Comparatively, China is making a rapid investment in research. The right way to focus on medical care is prevention. But if prevention is medicalized, it is just being used as another opportunity for the sale, which seems to be a big worry. For Instance:
- Diabetes is an epidemic. Incidence has been going up across the country. We all know one of the important reasons is lifestyle including diet. eg, a combination of western diet & Indian food is wreaking havoc. The answer is not medication; it is prevention. So more research should focus on a healthy diet, directing Government Policy to reduce obesity, rather that medicines.
- The number of people with non alcoholic fatty liver disease is going up. Its a new epidemic. A diet to reduce refined carbs and certain fats will reverse the condition, but currently a number of drugs are being taken through the licensing process. We Will be wasting precious funds on pills rather then prevention.
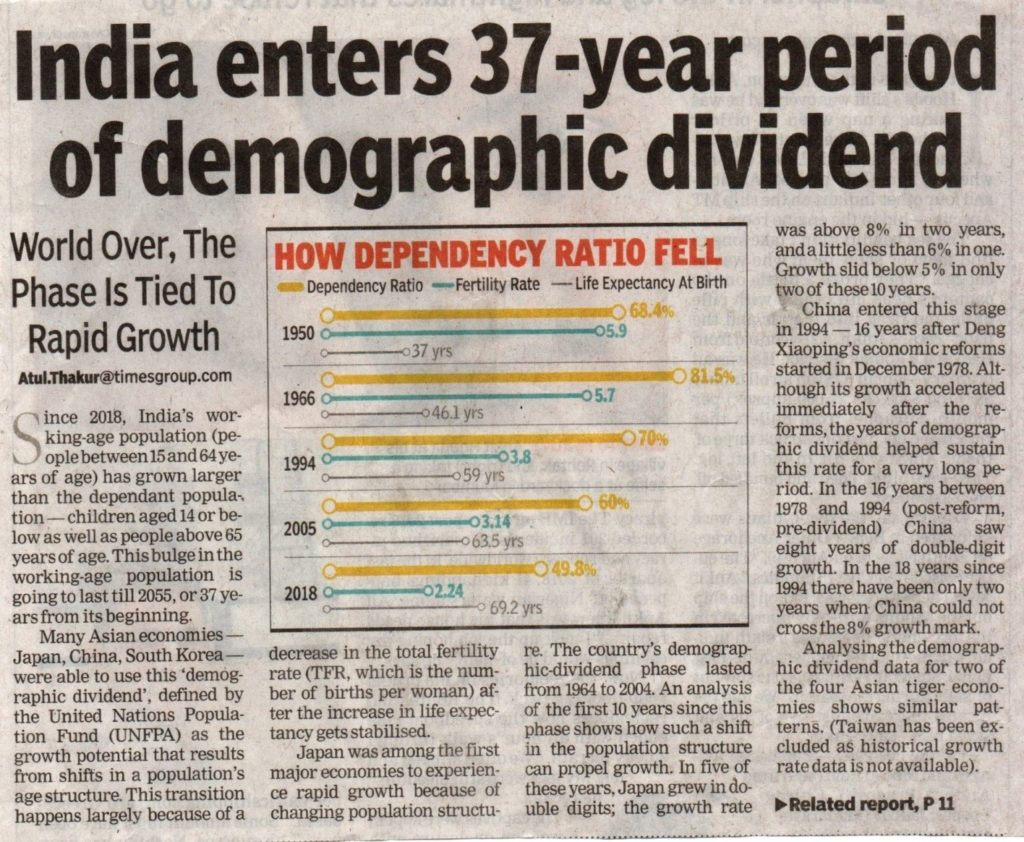
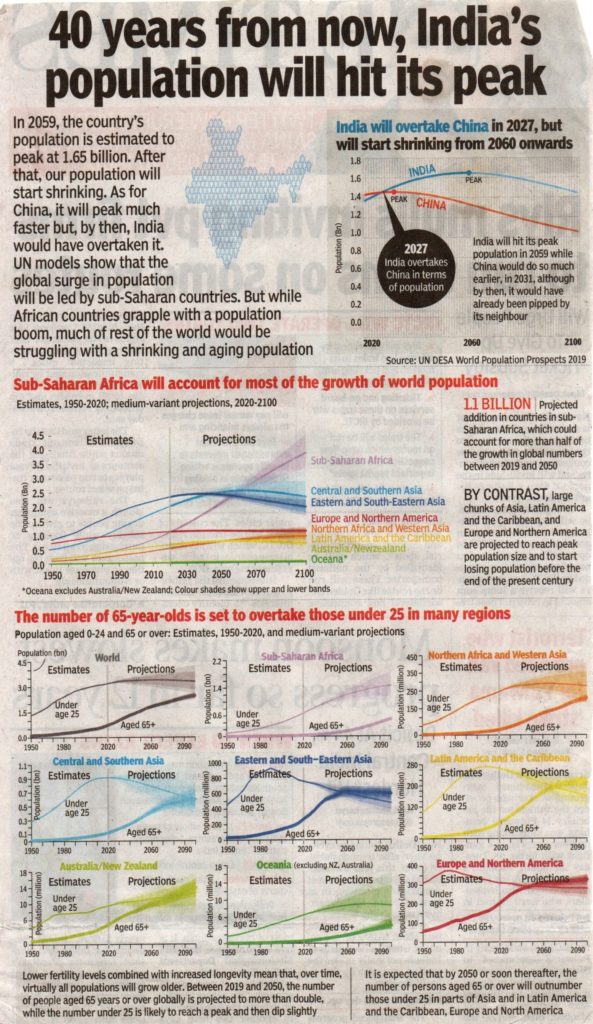
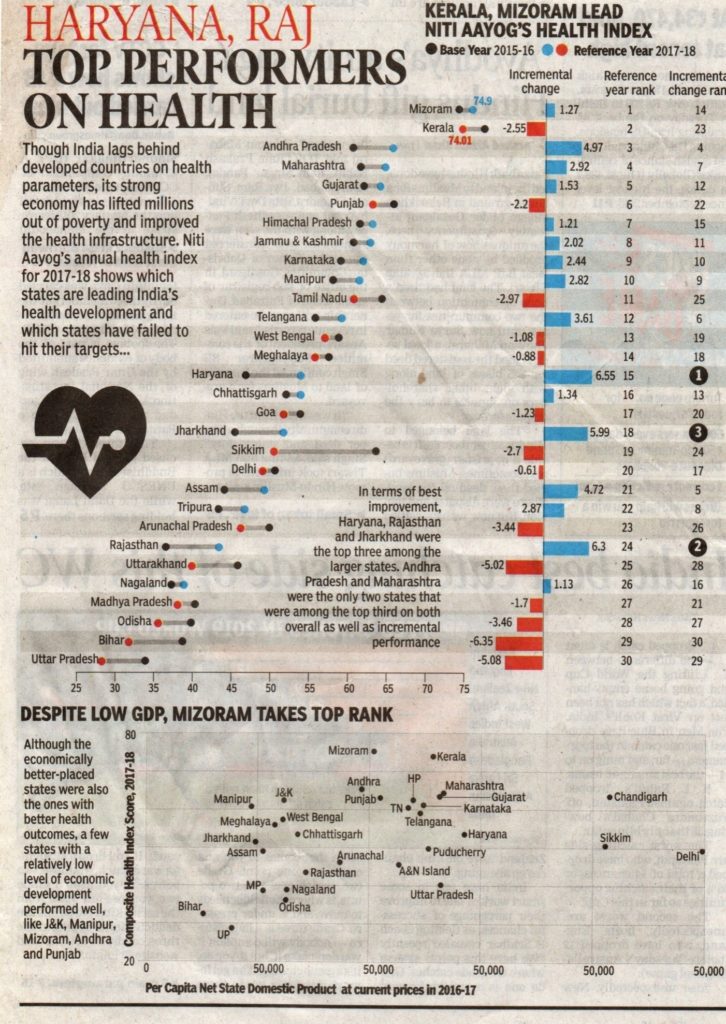
India’s current public health set-up is often traced to the Bhore committee of 1946. The committee’s continued relevance signifies its foresight, and our inability to achieve its recommendations. For instance, it recommended setting up 75-bedded hospitals for a population of 10,000 to 20,000. The bed to population ratio, 70 years later, is 9 per 10,000.
The three-tiered government health centre model that forms the core of the National Health Mission (NHM), has evolved from the committee’s recommendations. There is a base of sub-centers (SC; covering 3,000 to 5,000 people) and primary health centers (PHC; covering 20,000 to 30,000 people) which are the first points of contact for the patient with the government health system. These centers are capable of a basic set of services, which includes conducting normal (vaginal) deliveries. If the patient’s needs are beyond the services available, she is referred to a higher centre which houses specialists.
These community health centers (CHC) cover 80,000 to 1,20,000 people, and have a physician, a gynecologist, a surgeon, and a pediatrician. For even more complicated procedures and diseases, the patient is further referred to district hospitals (DH; also called tertiary centers). This system of graded care with referral linkages helps to bring health and medical care close to a patient’s home and ensures timely treatment.
The network of this infrastructure comprises 1.5 lakh SC, 25,000 PHC, 5,600 CHC, and 760 DH. This still falls short of the population norms mentioned above, by 19-30%. While the brick-and-mortar gap should be plugged, it is worthwhile to take stock of whether these 2 lakh institutions are working efficiently. If they were, our Public Health Pyramid would not currently be balancing on its tip.
Studies show that more than 50% of patients at tertiary centers are only in need of primary care. One can also use this inverted pyramid to partially explain why so many patients choose to visit quacks, euphemistically referred to as rural medical practitioners (abbreviated as RMP, which is also the abbreviation for legitimate medical doctors: registered medical practitioners). The latest round of National Family Health Survey 2015-16 which had a sample of 5.7 lakh households, shows that the most common reasons for non-availing of services at government health centers are poor quality of services, no nearby health facility, and long waiting lines. To address these issues:
Firstly, the public healthcare system in India needs to build a reputation for credibility. SCs are being transformed into health and wellness centers (HWCs) under the Ayushmaan Bharat Program. This transformation will entail a reorientation of SC from beyond the historic focus on reproductive and child health (deliveries, immunisation, childhood diarrhea and pneumonia) to include non-communicable diseases, oral health, emergency medical care, etc. Measures to improve service delivery and not merely expanding its ambit are critical. A strong foundation of first-point-of contact centers will lessen the burden on specialist hospitals where much time and money are wasted.
Secondly, a humble acknowledgement of the limitations of the public healthcare sector needs to be made and an assessment of the complementarities of the Private sector should be done. While Niti Aayog has been encouraging states to take up a PPP model for setting up hospitals, the regulatory environment must also incentivise more single doctor clinics to plug the rural-urban inequality.
Thirdly, technology has been tested to improve access and its quality. Tata Trusts and the Karnataka government put forth the ‘Digital Nerve Centre’ which merges the last two suggestions. It uses tele-medicine, video-conferencing and e-appointments systems to improve patient’s experience. While there may be limitations in its scalability, such innovative interventions need to be tried out across the country.
With government spending on health stagnating at 1% of GDP, capacity building of the existing institutional framework will be a challenge. Much hinges on creating an ecosystem of partnership and innovation which brings to the fore a renewed vigor for improving India’s healthcare system.
Patient – doctor relationship has to strengthen; patients should trust doctors. One can also say that doctors need to instill faith in their patients. Doctors in government hospitals are par excellence, so is the support staff. Their skills are exemplary; especially when you look at the number of patients they attend to on any single day. Medical staff, including doctors, is extremely overworked. In such situations, paying attention to enhancing doctor-patient trust sometimes takes a backseat.
A skewed doctor-patient ratio in our country is the major cause of trouble. In almost all leading countries of the world a doctor in a government hospital checks a maximum of 30 patients a day. In India, any doctor on average checks at least 150 patients a day. Number of relatives exceed the number of patients, leading to more crowds and ruining hygiene standards. Immediate steps to be taken are an increase in the number of seats in government medical colleges and medical faculty, and strengthening primary and secondary healthcare facilities.
There is no differentiation between patients. We get primary, secondary and tertiary patients even from remote areas in the state. Government healthcare facilities in villages and taluka level or small towns need to be improved to correct this situation. It is important that the government makes concerted efforts in improving primary and secondary healthcare facilities.
The academic stress and workload is higher in medical courses, especially in government medical colleges. That is why some students are unable to cope with the stress. They need to be taught certain soft skills from the beginning and some techniques to boost their emotional quotient as well. This training will surely help them. Life is tough, more so for a doctor. A good doctor has to learn to cope with the challenges of this profession efficiently
“Work for a cause, Not for Applause,
Live life to express, not to impress,
Don’t strive to make your presence noticed,
Just make sure your absence felt.”
WHAT HOMOEOPATHY HAS TO OFFER?
Homoeopaths understand that dis-ease, the energetic imbalance within us all, is a complex issue, and one that can only be fully cured by using a remedy similar in its energy to that of the shock or trauma that caused the imbalance. By understanding the origins of dis-ease and how the symptoms of the imbalance show themselves to a careful observer, the homoeopath is able to help individuals cure themselves on a profound level. Also the homeopathic case taking process shows care and concern for the patient and it is this caring that is healing.
Homeopathic remedies are like miniature time-space bombs, which go to the blockage or disease and blow it up, thus releasing the stored energy and facilitating a cure. It is able to destroy these diseases because it is based on the natural law of cure, which is the application of medicines based on the Principle of similar. Essentially homeopathic medicine is an artificial disease that matches the energetic resonance of the disease of the patient, and the law of resonance states that two similar energies cannot co-exist, so they effectively destroy one another.
The origins of our dis-eases are ancient. At conception, we all are given a gift package (whether we want it or not!) that includes a predisposition (called a miasm) to all of the familial tendencies our ancestors have accumulated and exhibited over the years. These can be as simple as eczema or allergies, as serious as cancer, arthritis or heart disease, or as deep as a tendency toward alcoholism, depression, self-mutilation, eating disorders or suicide. They also are the origins of sexual cruelty, aggression, and violence.
Whether or not we see these predispositions come to light in our lives, has a great deal to do with our lives, the shocks and traumas to our system that, as Dr Samuel Hahnemann, homoeopathy’s founder, termed it, “…bow down the soul.” These traumas wear on our ability to stay balanced and whole, and make themselves known to us in any number of ways (often called symptoms), which homoeopaths see as an attempt by our life energy to communicate to us that there is something going on inside that needs to be dealt with.
” AAINA MUJHSE MERI PEHLE SI SURAT MANGE,
MERE APNE MERE HONE KI NISHANI MANGE………”
BIBLIOGRAPHY
- Shreemad Bhagwat Gita
- Organon of medicine and Philosophy – Dr Hahnemann
- Psyche and Substance – Dr Whitmont E.C.
- Preventive and Social Medicine – K. Park.
- A Comprehensive textbook of community medicine – Mathur.
- Textbook of Preventive and social medicine – Mahajan Gupta.
- Preventive and Social Medicine – Jana
- A textbook on hygiene and public health – B.N. Ghosh.
- Social and Preventive Medicine – Atmaram Bedi.
- Homoeopathic Preventive Medicine – Fredricke L. Compton.
- Health Education and community pharmacy – N. Murugesh.
- Texbook of community medicine – Rajvir Bhalwar.
- Practical Manual of Community Medicine – D. K. Mahabalaraju.
- Practical and Viva of Community Medicine – J. Kishore.
- Community Medicine with recent Advances – A. H. Suryakant.
- Mastering Practicals of Community Medicine – Purnima and Shashank Tiwari.
- Materia MedicaPura – Dr Hahnemann.
- Allen’s encyclopedia.



About the Author:
Dr PRIYANKA BHATT, B.H.M.S. M.D. (Mat med.) Lect. (Community medicine)
DIVA’S DIVINE HOMOEOPATHY, Pandit Jawahar Lal Nehru Homeopathic Medical College and Hospital, Kanpur