ABSTRACT:
Introduction: The term homoeoprophylaxis (HP) was first used by Burnett in 1884 to refer to medicines selected according to the Law/Principle of Similars to prevent targeted infectious diseases. HP medicines were first used by Hahnemann in 1798 and have been used since to protect significant numbers of people against a range of infectious diseases in many countries. This paper uses the results of a recent analysis of large HP interventions to assess the potential value of HP in epidemic and endemic conditions.
Methods: Using a previous analysis as a starting point, the potential value of HP in different conditions is considered.
Results: Thirty-four annual HP interventions were noted in India, Cuba and Brazil. When counted by a person, by disease, and by year, over 250 million people were covered by the interventions studied. The effectiveness of HP appears to range between 63% and 99% with a weighted average of around 90%. These results are consistent across endemic and epidemic use. The HP programs against Japanese Encephalitis and Acute Encephalitis Syndrome in Andhra Pradesh and Telangana, India, and against Dengue Fever in Macaé, Brazil, were found to provide new insights into the use of HP in both endemic and epidemic conditions.
Discussion: HP is used to prevent targeted diseases in large and small populations. Its use is often directed by government agencies and conducted by medical doctors and scientists. HP is potentially valuable, especially in situations where vaccination is not possible either due to there being no vaccine for the disease, or when an existing vaccine cannot be obtained in sufficient quantities, or in time to treat an outbreak. But it also has potential value in all other situations where immunisation is required.
Conclusion: There are proven benefits from the widespread use of appropriate HP interventions, including saving lives and preventing suffering. HP can provide governments with a very economical practical option to combat infectious diseases in both endemic and epidemic situations.
KEYWORDS: homoeoprophylaxis, epidemic, endemic, immunisation
CONFLICT OF INTEREST: The author declares that he consults parents regarding immunisation options, including homoeoprophylaxis.
FINANCIAL SUPPORT: The author has received no funding for this project.
Introduction:
Homoeoprophylaxis (HP) is defined as the systematic use of potentized substances selected using the Law/Principle of Similars and administered using the Law/Principle of Minimum Dose to prevent the development of the characteristic symptoms of a targeted infectious disease in previously unprotected persons (i.e. have not had the disease nor used vaccination or HP).
Burnett first used the term Homoeoprophylaxis in 1884 saying “ that likes are prevented by likes, I could adduce very many examples to show”, and that HP is “the prevention of disease according to the law of similar”[1]. Dr Samuel Hahnemann first used Belladonna 30 to prevent Scarlet Fever in 1798[2], and later suggested three remedies to prevent Cholera.[3] Since then HP has been used to prevent most infectious diseases in most countries[4],[5],[6]. However, it has only been in the last 15 years that the evidentiary base of HP has been significantly developed.
It is probable that many HP interventions have not been documented because they are often undertaken in emergencies which require an immediate practical remedy distribution, and where meticulous pre-planning and highly organised record-keeping are secondary to saving lives and suffering [7]. However, a recent analysis has documented a substantial evidentiary base for HP which can be used to draw new conclusions regarding the potential value of HP in epidemic and endemic conditions.
Methods:
A recent analysis published in the American Journal of Homeopathic Medicine(AJHM) documented the use of HP in over 250 million people on an annualised basis in three countries[8]. It included new information about the use of HP to immunise against Japanese Encephalitis (JE) and Acute Encephalitis Syndrome (AES) in Andhra Pradesh and Telangana States. An extension to the previous JE program was identified and described.
Data concerning JE and AES from 1997 to 2017 was sought, and a variety of relevant sources were identified[9]. Trends were calculated.
Confounding factors were recognized: (1) in July 2014 Andhra Pradesh was separated into two states, with a new state Telangana being formed. Hence the data series had to accommodate this change, (2) data regarding JE and AES was originally combined but has been shown separately from 2008 onwards. Some AES cases are caused by JE and some are not, making data classification difficult [10]. However, since HP is based on the Principle of Similars, and the symptoms of JE are similar to AES, the HP program against JE would have some benefit against AES because of this similarity.
In order to provide as much consistency in the data trends as possible, the data for JE and AES was combined, as were the results for Andhra Pradesh and Telangana States.
Results:
The HP interventions undertaken in three countries, and summarised in Table 1, were described in detail elsewhere[11] . Many more examples of HP interventions both in these and in other countries exist[12].
The quality of analyses into the HP interventions listed is variable. Some interventions were controlled, but none were randomised. Sometimes Nosodes (N) (homeopathic preparations from diseased material) were used, and sometimes Genus Epidemicus remedies (GE) (homeopathic preparations of remedies used to treat the targeted disease).
Methods used to measure the effectiveness of results also is variable. Table 1 shows the classification scheme used in Table 3 to provide readers with a guide to the methodology used in each intervention.
Table 1: Classification of Effectiveness
| Code | Description |
| Statistical | |
| A | Direct control group |
| B | Indirect control group [13] |
| C | Simple % of cohort studied |
| D | Historical trend of actual reports |
| E | Fall factor analysis [14] |
| F | No control or historical trend |
| Descriptive | |
| G | Clearly positive result |
| H | Somewhat positive result |
| I | Unclear result |
| J | Negative result |
| K | Results not yet published |
The lack of homogeneity of studies as well as the variable quality of analysis makes a reliable meta-analysis of data problematical. However, there is consistency among reports quantifying effectiveness (which ranges between 63.9% to 99.96% with a weighted average after removing the highest and lowest readings of 89.45%). This reinforces the value of the overall findings, as does the fact that these interventions are “real world” responses to urgent needs, rather than academic studies.
It was noted whether the interventions were directed by Government agencies, undertaken by Government accredited Institutes or Universities, or undertaken by private practitioners. The prophylactic method used was recorded.
Table 2: Major HP Interventions in Three Countries
| Year | Disease | Numbers | Government directed | Type/Dose | Effectiveness (%) |
| CUBA[15] | 25,020,000 | ||||
| 2007 | Leptospirosis | 2.2 million | Yes, via Finlay Institute | N | B. |
| 2007 | Hepatitis A | 1 million | Yes, via Finlay Institute | N | D. |
| 2008 | Leptospirosis | 2.2 million | Yes, via Finlay Institute | N | B. |
| 2009 | Dengue Fever | 20,000 | Yes, via Finlay Institute | N, GE | A. 74.1% to 100.0% |
| 2010 | Swine Flu | 9.8 million | Yes, via Finlay Institute | N | D. |
| 2010 | Pneumococcal | 9.8 million | Yes, via Finlay Institute | N | D. |
| INDIA | 224,718,447 | ||||
| 1989 19911993 | Japanese Encephalitis[16] | 322,812 persons39,250 follow up | Yes, via CCRH | GE | 99.96% C |
| 1996 | Dengue[17] | > 39,200. Follow up 23,520 | Yes, via CCRH | GE | 99.97% C |
| 1999 -2009 | Japanese encephalitis[18] | 20,000,000 per annum 14 years and younger | Yes, Government Department of Indian Medicine and Homoeopathy. | GE+N+constitutional | B, D |
| 2006 | Chikungunya[19] | 1061 HP563 control | No, post-grad doctors at Government University | GE 200 t.d.s for 5 days | 75.7% A82.19% C |
| 2007 | Epidemic fever[20] | Distributed to 1,855,374 In 8 wards. | Yes, Kerala government’s RAECH program. Average intake 58.86%6,602 surveyed. | GE | 63.9% A 73.83% C |
| 2012 | Dengue[21] | 2,500,000 | Yes, Medical and Health Department, Chittorr, | GE | K |
| BRAZIL | 870,698 | ||||
| 1974 | Meningococcal[22] | 18,640 HP6,430 no HP | No, private doctors | N. 1 dose | 95% A |
| 1998 | Meningococcal[23] | 65,826 HP23,532 not HP | Yes, government-funded study, conducted by two Professors of Medicine from the University Foundation in Blumenau, Brazil, and a Blumenau specialist physician and Health City Secretary. | N | 95% 6 mthsto91% 12 mths A |
| 2001 | Dengue[24] | 1,959 | No, private doctors | GE 30. 1 dose | 81.5% B, EInferred rate |
| 2007 | Dengue | 7,300 people20,000 doses | Yes, Health Secretary Program, Sao Jose do Rio Preto | GE complex1 dose | G |
| 2007 | Dengue[25] | 156,000 people216,000 doses** | Yes, Secretary of Health of the municipality of Macaé, Rio de Janeiro, | GE complex1 – 2 doses | 86.7% BInferred rate |
| 2007 – 2012 | Dengue[26] | Doses *2007: 216,0002008: 203,878;2009: 211,059;2010: 178 677;2011 150,682;2012 125,621. | Yes, Secretary of Health the municipality of Macaé, Rio de Janeiro, | GE complex | 89.4% Binferred rate |
* The number of persons who used HP in the 5 years from 2008 to 2012 is estimated to be 628,273 using the ratio of doses to people shown in the 2007 intervention
** Not included in analysis as shown in following reference
If further details of each intervention are required then they are available in the earlier analysis noted above.
Table 3: Amended Summary of HP Interventions Listed
| Country | Programs by Years * | Interventions by Person, by Year and by Disease |
| Cuba | 6 | 25,020,000 |
| India | 18 | 224,718,447 |
| Brazil | 10 | 870,698 |
| 34 | 250,609,145 |
* each individual year of each program is shown. For example, the final Brazilian program which ran from 2007 to 2012 is counted as 6 years.
The amalgamation of JE and AES data from 1995 to 2017 in Andhra Pradesh and Telangana is reported in Table 4 and Figure 1. The figures in bold italics show where different figures were reported for the same time period in the different sources examined. The figures used were selected by the author as being the most reasonable estimate based on examination of results shown in the different sources. Variations between these different figures were not large and use of possible alternatives would not meaningfully change the results or conclusions.
Table 4: JE and AES Notifications and Deaths in Andhra Pradesh and Telangana states
| Andhra Pradesh | Telangana | Combined Andhra Pradesh, TelanganaJE and AES | ||||||||||
| Japanese Encephalitis | AES | Japanese Encephalitis | AES | |||||||||
| Year | Notif. | Dths | Notif. | Dths | Year | Notif. | Dths | Notif. | Dths | Year | Notif. | Dths |
| 1995 | 986 | 269 | 1995 | 986 | 269 | |||||||
| 1996 | 332 | 108 | 1996 | 332 | 108 | |||||||
| 1997 | 984 | 247 | 1997 | 984 | 247 | |||||||
| 1998 | 524 | 192 | 1998 | 524 | 192 | |||||||
| 1999 | 965 | 203 | 1999 | 965 | 203 | |||||||
| 2000 | 343 | 72 | 2000 | 343 | 72 | |||||||
| 2001 | 33 | 4 | 2001 | 33 | 4 | |||||||
| 2002 | 22 | 3 | 2002 | 22 | 3 | |||||||
| 2003 | 397 | 183 | 2003 | 397 | 183 | |||||||
| 2004 | 7 | 3 | 2004 | 7 | 3 | |||||||
| 2005 | 34 | 0 | 2005 | 34 | 0 | |||||||
| 2006 | 11 | 0 | 2006 | 11 | 0 | |||||||
| 2007 | 22 | 0 | 2007 | 22 | 0 | |||||||
| 2008 | 16 | 0 | 22 | – | 2008 | 38 | 0 | |||||
| 2009 | 35 | 0 | 49 | – | 2009 | 84 | 0 | |||||
| 2010 | 7 | 5 | 139 | – | 2010 | 146 | 5 | |||||
| 2011 | 4 | 1 | 73 | – | 2011 | 77 | 1 | |||||
| 2012 | 3 | 0 | 64 | – | 2012 | 67 | 0 | |||||
| 2013 | 7 | 3 | 345 | 3 | 2013 | 352 | 6 | |||||
| 2014 | 0 | 0 | 31 | 0 | 2014 | 0 | 0 | 155 | 5 | 2014 | 186 | 5 |
| 2015 | 0 | 0 | 50 | 0 | 2015 | 8 | 1 | 157 | 1 | 2015 | 215 | 2 |
| 2016 | 0 | 0 | 4 | 0 | 2016 | 4 | 0 | 72 | 0 | 2016 | 80 | 0 |
| 2017 | 1 | 0 | 37 | 0 | 2017 | 11 | 0 | 136 | 0 | 2017 | 185 | 0 |
Figure 1: Combined JE and AES Notifications and Deaths for Andhra Pradesh and Telangana
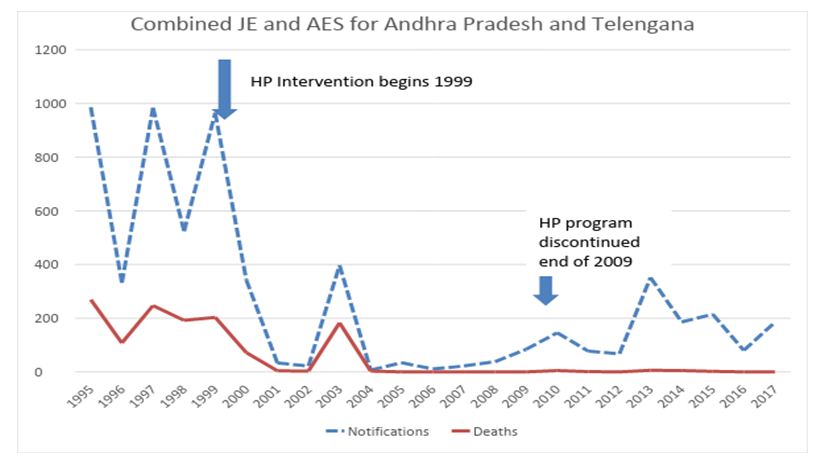
The spike in notifications and deaths from JE in 2003 appears to be out of sequence. The AJHM analysis examined different possibilities [27],[28],[29] and concluded that “it is uncertain whether the spike in 2003 is due to JE, and in one other analysis cited the 2003 rates were negligible .”
Table 5 shows the annual averages for notifications and deaths for JE and AES for the last 6 years of the HP intervention and 8 years after the intervention ceased. 2003 figures were excluded from the analysis due to the uncertainty noted above.
Table 5: Averages for Notifications and Deaths During and After the HP Intervention
| Annual Averages | ||||
| Years | # | Notifications | Deaths | |
| During intervention | 2004 – 2009 | 6 | 32.7 | 0.5 |
| After Intervention ceased | 2010 – 2017 | 8 | 163.5 | 2.4 |
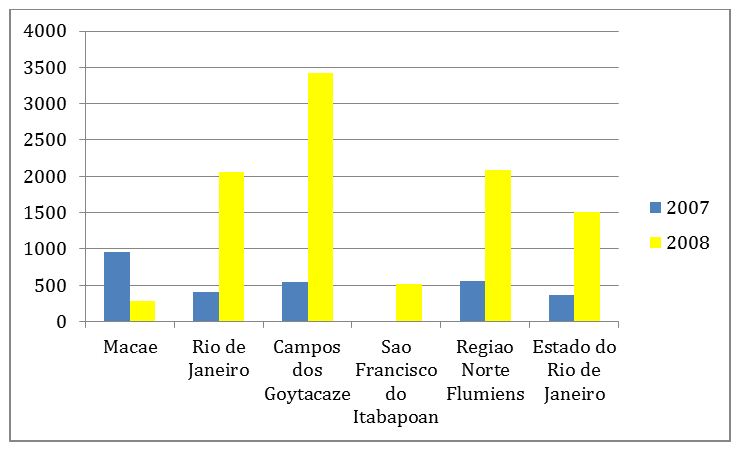
Another example of the use of HP over a number of years is shown in the Brazilian interventions against Dengue in Macaé, Rio de Janeiro, as described in Table 6 and Figure 2. In districts surrounding Macaé, the trend was clearly upwards, whereas in Macaé the trend was reversed.
Table 6: Dengue incidence coefficient by municipality, state and region, 2007-2008
| Incidence by 100,000 inhabitants | Macaé | Rio de Janeiro | Campos dos Goytacaze | Sao Francisco do Itabapoan | Regiao Norte Flumiens | Estado do Rio de Janeiro |
| 2007 | 961.79 | 411.26 | 538.45 | 14.65 | 558.23 | 361.93 |
| 2008 | 280.21 | 2,059.24 | 3423.5 | 520.67 | 2,081.19 | 1,503.19 |
Figure 2: Dengue incidence coefficient by the municipality, state and region,
2007-2008 (by 100,000 inhabitants)
Discussion:
Most HP interventions occur in rapid-onset epidemic situations. They are not academic exercises, but real-world interventions to save lives and suffering. However, both the largest Indian and the largest Brazilian interventions studied involved giving annual doses where the disease was endemic with seasonal increases.
The interventions in India against JE and AES in Andhra Pradesh and Telangana from 1999 to 2009 show that an annual program of HP against an endemic disease with seasonal increases can be successful. Each year in August children aged to 15 years was given the following protocol: Days 1,2,3 – Belladonna 200; Day 10 – Calcarea Carbonicum 200; Day 25 – Tuberculinum Kent M.
Data in Tables 3 and 4 and Figure 1 show that when the program was stopped in 2010 then over time there was a general increase in the incidence of the disease. This is unsurprising given that around 1.3 million infants are born in the two States each year from 2010 onwards who have not been protected by HP.
The annual interventions in Brazil in the municipality of Macaé, Rio de Janeiro from 2007 to 2012 were similarly successful.
This experience is somewhat similar to the author’s experience from 1985 to the present day using annual triple doses of indicated remedies against a range of endemic diseases in Australia (some of which also have seasonal increases), including Pertussis, Pneumococcal disease, Hib, Meningococcal Meningitis and Tetanus[30].
There is a degree of consistency across the HP interventions shown in Table 2, with a range of effectiveness between 63% and 99%. A weighted average of 89.45% is indicative of overall findings. These findings are consistent with the author’s long-term study from 1986 to 2002 where the effectiveness of HP was 90.4% (95% CI; 87.6% – 93.2%)[31].
Practical HP interventions show that appropriate HP programs[32] provide Governments with infectious disease options for epidemic and endemic diseases which are very flexible (potentially against any strains of infectious diseases), can be made rapidly available, have zero toxic side-effects, and are relatively inexpensive.
Appropriate HP programs offer travellers infectious disease options for similar reasons and may offer protection against diseases for which no vaccine is available (such as AES and Chikungunya).
The practical differences in prescribing for short-term/epidemic and long-term/endemic diseases – remedy selection, potency and frequency of doses – are discussed in detail elsewhere and are beyond the scope of this article[33]. However, the evidence above and in other studies suggests that HP effectiveness is similar for both short-term and long-term diseases[34]. Reactions to the remedies have not been collected in most interventions which, as stated above, are immediate responses to save lives rather than carefully prepared studies. The author’s study did collect data on reactions which occurred in less than 2% of doses and were typically brief and mild[35]. The safety of appropriate HP interventions allows treatment of every person in a cohort without the need for pre-screening.
Conclusion:
The ability of appropriate homoeoprophylaxis programs targeting specific infectious diseases to produce a significant level of protection has been confirmed the time and again in large HP interventions, some of which have been presented here. No one study is perfect, but together they reveal consistently positive results.
Appropriate HP programs using either nosodes, genus epidemicus remedies and/or a miasmic-GE approach (as used against JE and AES) have value against both epidemic and endemic diseases, and have the potential to save many lives, even more suffering, as well as giving individuals and governments a very safe, economical and practical immunisation option.
ACKNOWLEDGEMENTS: The author wishes to thank Dr Raj Kumar Manchanda, Director General of the Central Council of Research in Homeopathy (CCRH), Delhi, India, and Dr Anil Khurana, Deputy Director General CCRH, for their support and permission to access CCRH archives, Dr Conception Campa Huergo who as President of the Finlay Institute in Havana, Cuba until 2015, instigated that country’s use of HP, and Dr Gustavo Bracho who as Vice President of the Finlay Institute to 2015 led most HP interventions conducted by the Finlay Institute from 2007 to 2015, and Dr Srinivasulu Gadugu for his help with data collection.
LIST OF GRAPHICS AND TABLES LEGENDS:
Table 1: Summary of HP Interventions Listed
Table 2: Classification of Effectiveness
Table 3: Major HP Interventions in Three Countries
Table 4: Amended Summary of HP Interventions Listed
Table 5: JE and AES Notifications and Deaths in Andhra Pradesh and Telangana states
Figure 1: Combined JE and AES Notifications and Deaths for Andhra Pradesh and Telangana
Table 6: Averages for Notifications and Deaths During and After the HP Intervention
Table 7: Dengue incidence coefficient by municipality, state and region, 2007-2008
Figure 2: Dengue incidence coefficient by municipality, state and region,
2007-2008 (by 100,000 inhabitants)
[1] Burnett JC Vaccinosis and its cure by Thuja; with remarks on homoeoprophylaxis. 2nd edition 1897. B Jain Publishing. Delhi, 1996. Pages 95-97.
[2] Hahnemann S. The Cure and Prevention of Scarlet Fever. 1801. Lesser Writings. 1986. B Jain Publishing. Delhi. pp.369-385.
[3] Hahnemann S. Cause and Prevention of the Asiatic Cholera.1831. Lesser Writings. 1986. B Jain Publishing. Delhi. pp.753-756.
[4] Sankaran P (1961) Prophylactics in Homoeopathy. The Homoeopathic Medical Publishers, Bombay.
[5] Golden I. The Complete Practitioners Manual of Homoeoprophylaxis. 2012. Isaac Golden Publications. Gisborne, Victoria, Australia. Diseases shown in Table 10.3.1: Summary of Disease Characteristics, pp. 129-130.
[6] National Centre for Homeopathy. Homoeoprophylaxis: Human Records, Studies and Trials (compiled by Fran Sheffield). . (accessed 4/12/18).
[7] Whilst anecdotal, given that data was not collected, the author has been told of interventions both in Cuba and India where outbreaks of infectious diseases were responded to by local homeopathic doctors who provided prophylaxis as well as treatment, just as Hahnemann had done in 1798. He has also heard from homeopathic colleagues in Australia of local outbreaks of particular diseases being met with prophylaxis among the practitioners’ own patients. In recent times, government interventions have generally been documented, although with varying degrees of thoroughness.
[8] Golden I. Large Homoeoprophylaxis: Brief and Long-Term Interventions. American Journal of Homeopathic Medicine. Winter, 2019; 112(1): 31-36.
[9] Sources accessed to discover new data included (1) World Health Organisation. Guidelines for Prevention and Control of Japanese Encephalitis. Zoonosis Division National Institute of Communicable Diseases (Directorate General of Health Services). 2006; (2) Tiwari S, Singh RK, Tiwari R, Dhole TN. Japanese encephalitis: a review of the Indian perspective. Braz J Infect Dis. 2012 Nov-Dec;16(6):564-73. doi: 10.1016/j.bjid.2012.10.004. Epub 2012 Nov 8. (3) Japanese Encephalitis: Global Status, GIDEON Informatics Inc. https://www.gideononline.com/ ; (4) Government of India Data. Via http://www.ncdc.gov.in/ ; (5) personal contacts of the author.
[10] An excellent article summarising differences between AES and JE is Ghosh S. and Basu A. Acute Encephalitis Syndrome in India: The Changing Scenario. Ann Neurosci. 2016 Sep; 23(3): 131–133.
Published online 2016 Sep 9. doi: 10.1159/000449177.
[11] Golden I. Use of Homoeoprophylaxis in Three Countries. Similia. 2018; 30(1):23-27.
[12] National Centre for Homeopathy. Homoeoprophylaxis: Human Records, Studies and Trials (compiled by Fran Sheffield). . (accessed 4/12/18).
[13] A direct control group is where the control is part of a single cohort where an intervention against a targeted disease is being studied, e.g. a HP and a non-HP group within the same city, or same region. An indirect control group is where a single disease is intervened within say one State or one suburb, and notifications and deaths from the disease are compared to those in other States or suburbs.
[14] A fall factor analysis compares the rates of decline in the incidence of a targeted infectious disease in different regions or different cohorts within one region. These rates can be plotted to show a simple visual comparison.
[15] The pre-2014 Cuban interventions are summarised in Bracho G, Golden I. A Brief History of Homeoprophylaxis in Cuba, 2004-2014. Homeopathic Links. 2016; 29(2):128-134.
[16] Rastogi DP & Sharma VD. Study of homoeopathic drugs in encephalitis epidemic (1991) in Uttar Pradesh (India). CCRH Quarterly Bulletin 14(3-4) 1992. pp 1-11.
[17] CCRH. Dengue epidemic – Scientific activities of Council. CCRH News No. 23 (1996-97). pp 10.
[18] Srinivasulu Gadugu, Srinivasa Rao Nyapati, , G.L.N. Sastry An open observational study on efficacy of miasmatic prescription in the prevention of Japanese Encephalitis. Homeopathy. January 2014. Volume 103, Issue 1, Pages 78–79.
[19] Dr R Rejikumar, Dr R S Dinesh etal. A Study on the Prophylactic Efficacy of Homoeopathic Preventive Medicine Against Chikungunya Fever. http://www.similima.com/pdf/efficacy-chiunguna-kerala.pdf
[20] Protective Efficacy of “Genus Epidemicus” (Homeopathic Preventative) Administered During Epidemic Fever in Kerala http://www.homoeopathy.kerala.gov.in/docs/jan2011/raech_report.pdf
[21] The Hindu: Homeopathy to fight dengue fever http://www.thehindu.com/todays-paper/tp-national/tp-andhrapradesh/homeop…
[22] Castro, D. & Nogueira, G. G. (1975). Use of the nosode Meningococcinum as a preventative against meningitis. Journal of the American Institute of Homeopathy, 1975 Dec 68 (4), 211-219.
[23] Mronisnski C, Adriano E & Mattos G. (1998/99) Meningococcinum: Its protective effect against Meningococcal disease, Homeopathic Links, Vol 14 Winter 2001, 230-234.
[24] Marino R (2008). Homeopathy and collective health: The case of dengue epidemics. International Journal of High Dilution Research; 7(25): 179-185
[25] de Souza Nunes LA (2008). Contribution of homeopathy to the control of an outbreak of dengue in Macaé, Rio de Janeiro. International Journal of High Dilution Research; 7(25): 186-192.
[26] Dengue and Homeopathy: a successful experience from Macae http://www.ecomedicina.com.br/site/conteudo/entrevista22.asp
[27] John TJ Outbreaks of Killer Brain Disease in Children: Mystery or Missed Diagnosis? Indian Pediatrics 2003; 40:863-869.
[28] Rao MN. Outbreak of Killer Brain Disease in Children. Indian Pediatrics. Volume 41. January 17, 2004.
[29] Rao BL, Basu A, Wairagkar NS et.al. A large outbreak of acute encephalitis with high fatality rate in children in Andhra Pradesh, India, in 2003, associated with Chandipura virus. The Lancet. 364 (9437), 2004; 869-874.
[30] Golden I. The Complete Practitioners Manual of Homoeoprophylaxis. 2012. Isaac Golden Publications. Gisborne, Victoria, Australia. pp. 27-35.
[31] Ibid. pp. 63-68.
[32] Not all HP programs are appropriate. For example, Ibid pp. 35-37.
[33] Golden I. Ibid. Chapter 3. Short Term Homoeoprophylaxis in Practice. Chapter 4. Long Term Homoeoprophylaxis in Practice.
[34] Golden I. Ibid. Chapter 5. The Effectiveness of Homoeoprophylaxis.
[35] Golden I. Ibid. Chapter 6. The Safety of Homoeoprophylaxis.